Dr. Tom Frieden Blog: Covid Epidemiology
by Dr. Tom Frieden
Why I'm Optimistic
January 30, 2022
We have better tools, more information, more experience, and the best chance to save make the world a safer place than ever in our lifetimes.
Yes, there could be a deadly, transmissible, immune-escape Covid variant. But even in that worst-case scenario, we'd be far better prepared to handle it. And, it's likely that our immunity will continue to protect us, at least somewhat and likely to a signficant degree, from severe illness.
Better tools:
Immunity from vaccines and prior infection. Many highly effective vaccines, with billions of doses given. Not so effective against infection, but the most important goal is to prevent severe illness. We need to know more about how to prevent and treat long Covid, but we already know that if you don't get Covid, you don't get long Covid, and if you get Covid and are vaccinated, you're far less likely to get long Covid.
Treatments. Although they won't save nearly as many lives as vaccines, new treatments can prevent severe Covid, prevent hospitalizations, and prevent death. We're taming this virus.
Masks. Better masks are better, and there are now more of them. Back in 2009, I suggested that the U.S. learn from East Asia and mask up if we have to go out and are
Feeling sick;
Medically vulnerable;
Just concerned (or want to keep our noses warm in the winter or not sunburned in the summer :-) ... cycling around NYC I use a mask for those reasons)
Masking in this way would prevent many hospitalizations from influenza and other viruses, as would washing or sanitizing our hands more often.
Tests. Which we can use if feeling sick or before gathering when Covid is spreading.
Ventilation and filtration. Used correctly, ventilation and filtration can provide an important added layer of protection.
Better genomic surveillance. We're more likely to have an early warning if a nightmare scenario from this or another virus emerges. We're less vulnerable to a microbial sneak attack.
We have the opportunity to make the world much safer from health threats, including through commitment to find, report, and stop outbreaks promptly:
And we have growing commitment to strengthen WHO as a core anchor of our global health architecture and provide substantial resources to the Global Fund to support country improvements in preparedness:
Far, far too many lives have been lost to Covid, and it's not over yet. But we can learn the lessons from the past two years and work together to create a safer world where, instead of adding to fear of contagion, the connections among us strengthen our health, our economy, and our common community.
What Will the Next Few Months Look Like? Your Covid Questions, Answered.
We need to maximize control of the virus while minimizing harm
ovid has changed the world as we know it, and virulent variants such as Delta have upended early hopes of a clearer-cut “back to normal.” Unfortunately, achieving herd immunity may now be an impossible dream, but we can limit death and disruption as we get to a new normal.
Although the Delta-fueled wave in the United States is receding, Covid continues to spread globally and in many unvaccinated parts of the U.S. The reality is that many places around the world will continue to struggle with clusters and outbreaks until vaccine production is ramped up substantially. Until we can vaccinate the world, it’s up to us to deploy simple protection measures to control spread. I recently wrote in the Wall Street Journal about how we need to maximize control of Covid while minimizing its harm to our societies and economies.
The good news, at least in the U.S., is that just over 186 million — 76% of those eligible — are now fully vaccinated against SARS-CoV-2. This means that most of us have more freedom to do things that we used to do. But the truth is that the “new normal” will be different. This includes the way that we socialize and travel, the precautions we take, and how we move in public settings.
I’ve tried to address some of the most common questions about what the next few months and years may look like. One caveat: no one knows with certainty what will happen with Covid, and with our response to it. It’s conceivable that the virus could become less deadly and the pandemic could fizzle globally. It’s also conceivable that vaccine-escape variants could emerge and spread, setting the global fight back a year or more. Some questions can be answered, at least as of what we know in mid-October 2021, so here goes.
Should I get a booster shot?
Boosters are likely to benefit those for whom they’re recommended, including those at higher risk for severe disease such as the immunocompromised and elderly. We still don’t know if the Delta variant causes more severe disease, or whether immunity wanes significantly enough over time to warrant a third dose. Only time will tell if a third dose will be part of the full vaccine regimen for the entire population.
But it’s important to note — the reason we continue to see so many hospitalizations and deaths is that there are still nearly 70 million people in the U.S. who haven’t yet started their vaccination series.
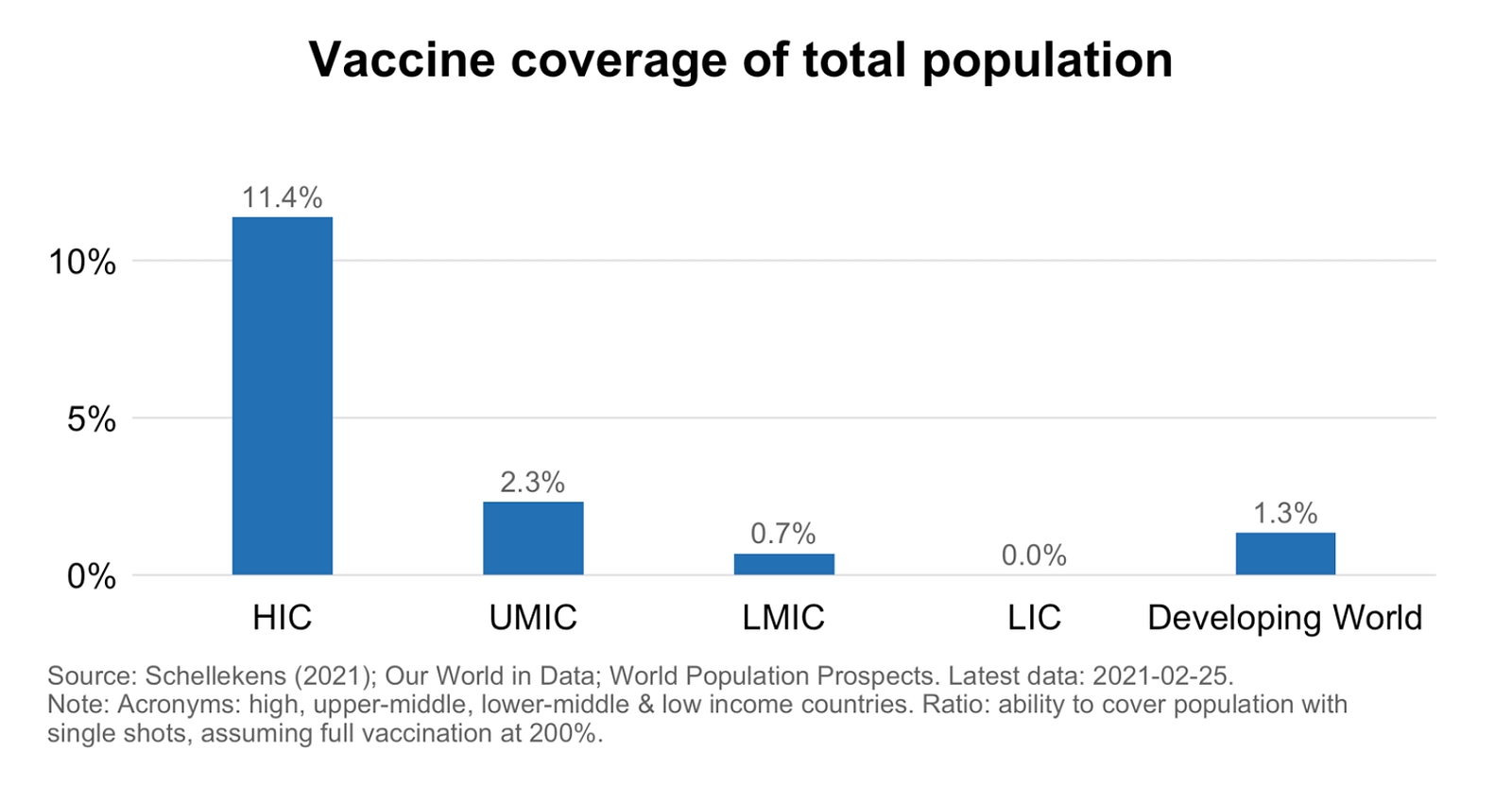
The issue of booster doses also raises questions of vaccine equity. In many countries including the U.S., people will get their third doses long before healthcare workers and at-risk populations in Africa and elsewhere are able to receive their first. It’s another reason we need to ramp up production and distribution globally, and fast.
Do I still need to wear a mask, and for how much longer?
I previously wrote a Medium piece on masking. In short, there are three factors to consider about masking: who you are, where you are, and what you’re doing. Much as we may dislike it, continued masking is important for certain people and in certain situations. Those who are at higher risk for severe disease or live with those who are at higher risk, live in an area with high spread, or are taking part in a risky activity should consider masking up to protect themselves and those around them.
Consider upgrading to an N95 or KN95 mask, especially if you’re at high risk of severe Covid disease, are around someone who is, or around a lot of unvaccinated people. Not all masks are created equal, nor do they protect against Covid equally.
It’s likely that masking will be with us for the long run for certain situations. This doesn’t have to be a bad thing. Masking helps control the spread of other infectious diseases, including the seasonal flu which kills tens of thousands each year. Wearing a mask doesn’t just have to be a pandemic practice — it could become a social norm, as it is now in parts of Asia, that helps control the spread of various diseases and keeps us all healthier.
When will it be safe to resume normal activities such as taking public transit, or going to restaurants and the gym?
The truth is that every action we take has risks associated with it. Even something as basic as drinking a glass of water can present a risk. Some activities are riskier than others.
If you’re fully vaccinated, there’s a lot you can do safely now, with a few exceptions. Ultimately, it comes down to the levels of spread in your community and the risk to yourself and those you live with.
If you are vaccinated and need to take the subway to get to work, there’s a risk — we don’t know how high a risk — of infection. You’ll be safer and can minimize the risk by wearing a higher-grade mask such as an N95/KN95. But if you live in an area where there is a high incidence of Covid, you could well get infected if you go into a crowded gym or restaurant.
The best way to feel confident about resuming normal activities is to get vaccinated. Even with breakthrough infections, those who are vaccinated have much less severe illness. To minimize risks and be on the safer side, consider employing additional layers of protection, such as ventilation, masking, and distancing.
Is gathering for family events and holidays like Thanksgiving going to be safe?
Risks associated with gatherings such as Thanksgiving have to do with how likely participants are to have been infected, how vulnerable people are, and what they are doing. The CDC has provided recommendations on what we can all do to make Thanksgiving safer. Just as with any activity, the best way to minimize risk is to make sure that you and those around you are vaccinated, then take extra precautions to reduce further possibility of infection.
Wearing masks when not eating (including N95/KN95 masks for anyone older, vulnerable, or simply worried), opening windows to increase ventilation, and limiting exposures in the days before any gathering can reduce the risk that Covid is an uninvited guest to your Thanksgiving get-together.
The Biden Administration recently announced it would spend $1 billion to increase the supply of at-home rapid tests. Encouraging anyone who’s had a lot of potential exposure (such as college kids, those who work in high-risk settings, or people who have recently travelled) to test beforehand will act as another tool in our arsenal to minimize risk.
It’s really about risks and benefits — and we have the tools to decrease the risks.
What’s next? How long will the pandemic continue?
The honest answer to this question is: no one knows.
One likely scenario is that we continue to see flare-ups and outbreaks, especially in places with high-risk populations such as nursing homes, prisons, homeless shelters, and camps. But with vaccines and, to a much lesser degree, therapeutic treatments, the virus will be tamed and won’t cause nearly the death and destruction it causes now.
A better scenario would be much lower transmission; worse would be a new variant that evades immunity. In any case, there are important layered protection measures on top of vaccination — including masking, testing, ventilation, and distancing — that we can take. People with compromised immune systems may want to be even more rigorous about taking these precautions.
Unfortunately, Covid is likely here to stay. What doesn’t need to be here to stay are the restrictions and the fear we’ve been living with. By adapting our individual and societal behaviors, we can protect ourselves and our communities and advance into a vaccinated, safer new normal.
This piece was orginally posted on Medium.
Don’t be blinded by the light at the end of the pandemic tunnel
Even as the United States moves closer to resuming life as usual, the end of the pandemic is far away for the rest of the world. Vaccines won’t crush the global curve in the short term, but protective measures work, as I discuss in a new op-ed for CNN. Globally, effective action can save more than a million lives in the coming year.
India’s explosive outbreak of Covid is a reminder that most of the world still faces ongoing and increasing risks of the pandemic, driven by variants that are more contagious and likely also deadlier. While some Americans are getting ready to go to the movies, body bags are stacking up in other parts of the world where vaccines aren’t available.
Vaccines won’t do much to stop uncontrolled spread in the short term. We don’t have enough of them, our vaccine infrastructure can’t be relied on to produce enough vaccines for the world, vaccines take months to roll out, and vaccine-induced immunity takes weeks to months to develop. So, in the short term, places such as India and Brazil can save the most lives by improving masking and distancing, and reducing travel.
mRNA vaccines are our insurance policy against variants, the possible need for boosters, and production delays with other vaccines, but current capacity is nowhere close to where we need it to be. Immunity from vaccines is at best months or years away.
We need to transfer vaccine technology and ramp up manufacturing now.
Right now, these are six key steps we must take to deal with outbreaks: 1. Protect health care and health care workers 2. Mask up 3. Maintain distancing to avoid superspreading 4. Continue essential services, including school 5. Vaccinate, especially health care workers and older people 6. Learn and adapt
The situation in India shows the urgent need to keep variants at bay through swift and strategic action. Global cooperation is essential if we are to win our war against Covid. It’s possible to beat this virus.
Benefits, Risks, and Future of Vaccines and the Pandemic
Look at it this way – this week, we learned that our vaccine safety monitoring system works. Reports that a small number of people developed a rare form of blood clot after receiving the Johnson & Johnson vaccine led to quick investigation, quick action, and transparency about what is known, not known, and what our next steps should be. Vaccines remain our way out of the pandemic.
Global collaboration has been critical throughout the pandemic. Public health and medical experts around the world are collaborating to determine whether events associated with AstraZeneca vaccine are the same as those which may be associated with the J&J vaccine.
Vaccine technology transfer
The pandemic is the world’s most important problem, making technology transfer for vaccines increasingly crucial. Right now, mRNA vaccine technology is our best solution. We need to create high-quality manufacturing platforms around the world to improve vaccine access. mRNA technology is an insurance policy against the pandemic.
mRNA vaccines are easier to tweak for vaccine-escape variants, less subject to production delays, and easier and quicker to bring to scale. They may be more effective against infection, and may be safer also. ALL licensed vaccines are safe and effective, but mRNA is the most promising technology.
We also need more efforts like Moderna’s to study vaccine thermostability at non-freezing temperatures and other efforts that may help get mRNA vaccines to places and communities that are harder to reach.
Public health success story
Vaccines are one of the most important public health interventions ever, having saved at least a billion lives. As with any medical intervention, there may be a small risk. The story of vaccines against rotavirus, which causes deadly diarrheal disease in young children, is instructive.
In 1999, the RotaShield vaccine was withdrawn from the US market because of a rare, serious complication. Other countries followed suit. This decision led to literally millions of preventable child deaths around the world until a new vaccine was developed 7 years later.
There’s still a low risk of serious complications associated with the newer rotavirus vaccines, but benefits of vaccination FAR outweigh the risks. Thus the US and around the world continue vaccinating children against rotavirus, looking carefully for possible complications, and saving millions of lives.
Vaccine risks vs. benefits
Even as rare but serious events possibly associated with the J&J vaccine continue to be investigated, the pandemic is continuing – and accelerating in much of the world. About 1 in 200 people with Covid die from it. There have so far been 6 reports of blood clots developing in the brain among almost 7 million people who received the J&J vaccine. There are no known reports of such events associated so far with the Pfizer or Moderna vaccines.
Analysis of risks and benefits guides recommendations for vaccines, including against Covid. This can be uncomfortable. We weigh “sins of commission” more heavily than “sins of omission.” But if every vaccine helps many thousands more people than it may harm, isn’t this the way to go?
Globally, until there is much more widespread availability of mRNA vaccines, benefits of use of the vectored vaccines will far outweigh risks in all communities in which Covid is spreading and for all populations at high risk of complications of Covid.
Vaccinating toward the new normal
The more people who are vaccinated with available vaccines, the lower the case rates, the more lives saved, and the sooner we will get to the new normal. I still think we’re likely to crush the curve of infections by summer and be in the new normal in the fall in the US.
We must balance the immense risks posed by Covid with extremely low risks of getting vaccinated. Fundamentally, the case for scaling up mRNA vaccine platforms globally just got even stronger than when we advocated for this 6 weeks ago.
Scaling up production of mRNA vaccines won’t be simple. Life rarely is. Technological transfer of the most promising vaccine technology against Covid isn’t just the right thing to do altruistically, it’s essential to the health and safety of every person, everywhere in the world.
###
Our Fundamental Challenge: Getting Vaccine Where It’s Needed Most - 4.13.21
The US vaccination campaign is facing a fundamental challenge: getting the vaccine where it’s needed most. Millions of Americans are still unprotected, many of them at high risk of severe illness. Our 4th surge is beginning. Lives are at stake.
As reported by @CDCgov in its Covid Data Tracker, 1 in 3 people in the US have received at least one dose of vaccine—but that means 2 in 3 haven’t. Millions of people age 50-64 and 65+ who haven’t yet been vaccinated can still get Covid and are at much higher risk of severe illness or death, especially with rapidly increasing spread of new variants.

More than 45 million still at high risk
There are still 12 million people age 65 and older who remain unvaccinated. Nearly half of those between 50 and 64 have been vaccinated, but that leaves 34 million in that group who haven’t been. Those not yet vaccinated are disproportionately Black and Latinx. We must do better.
The most prevalent strain of Covid in the US now is B117. This variant is more contagious and likely more deadly. How bad the 4th surge gets depends more on us than on the virus. New variant, but the same response is needed: vaccinate, mask, distance. Patience, discipline, solidarity.
In the coming weeks, we need to shift our strategy. It’s not enough for everyone to be eligible for vaccination, we have to make sure that people actually get vaccinated. That means reaching people at the highest risk of severe illness and death, and in the places with the most spread.
Aiming better
If we optimize vaccine distribution we can save the most lives. I explained last week how a single well-targeted vaccination could save 10 times more lives, and prevent 100 times more cases, than vaccinating a low-risk person in a low-risk community.
The number needed to vaccinate (NNV) to save one life shows impact of vaccines in high- vs. low-risk groups. Vaccinating anyone helps, but for the next 1-2 months, focusing on the highest-risk populations can save many more lives. We need to aim our shots better.
There have now been about 560,000 Covid deaths in the US: that’s 1 of 586 Americans. To prevent one death we need to vaccinate 586 people a year. Vaccinating 100 million people will save more than 170,000 lives from Covid this year (many more when secondary cases prevented are included in the calculation).
This is even more dramatic when we look at nursing homes. Roughly 220,000 nursing home residents have died from Covid. To prevent one death, we need to vaccinate around 7 nursing home residents, so vaccinating 1 million in this population alone will save 140,000 lives. Pretty amazing!
But focusing on age alone isn’t enough—we also have to improve vaccine equity by race and ethnicity. @KFF data shows a consistent pattern: Black and Hispanic people are less likely to be vaccinated even though they’re more likely to get Covid and die from it.

A preprint study showed we can save many more lives if we prioritize high-risk areas rather than focusing solely on age.
Right now, Michigan is being hit hard. Other states may follow. As hotspots emerge, we should flood the zone with vaccines. We also need to continue to mask up and take other measures, such as closing bars and limiting indoor dining at restaurants until vaccine coverage increases or cases decrease.
Make vaccination easy
There’s a lot more we can do to improve equity and overcome vaccine hesitancy. Make it easy to get vaccinated. Convenience overcomes reluctance. Instead of requiring appointments, let people walk in—especially those at high risk of severe illness and who demonstrated that they live in places with extensive spread. Offer extended hours, allow time off from work, and provide transportation to vaccination sites. Make vaccines widely available at doctors’ offices. Provide translation and call centers.
Reach people where they are. That means getting creative with mobile and non-traditional vaccination sites such as churches, schools, corner stores, bars, and pop-ups at community events. Use the right messages and the right messengers. Partner with community organizations and leaders.
Ask your friends, family, and neighbors if they've been vaccinated. If they haven’t been, ask if you can help them sign up, drive them to a vaccine clinic, or otherwise support them to get vaccinated. Listen to them and acknowledge their concerns, address these concerns with facts, and tell real stories of real people who have been harmed by Covid and those who are now protected by the vaccine.
We must do better with focused, rapid vaccination in the US. And we must recognize that global vaccine equity is an urgent crisis. Increasing manufacturing is the only way forward. As long as the virus is still among us, it’s a threat to all of us.
The Centrality of Equality
There’s lots of good news to report on vaccines, but the virus and variants are gaining ground. Variants are spreading rapidly in the US, driving (along with premature opening) the fourth surge that’s now underway. Here, I’ll explain why equity is not just about fairness, but essential for pandemic control.
I had planned to stop these weekly analyses, but couldn’t help sharing thoughts on this week’s developments – there have been so many.
The fourth surge is here
The feared fourth surge is building. CDC reports in its Covid Data Tracker Weekly that cases are up more than 8% nationally over the past week, and test positivity rates have risen slightly, to 5.1%. The situation in Michigan, which now has the highest rate of new cases of any state over the past seven days, is getting worse – and other states are at high risk of following this trend.
Vaccines – light at the end of the tunnel
The news on vaccines just keeps getting better. A CDC study of mRNA vaccines published in this week’s MMWR found that both the Pfizer and Moderna vaccines blocked 90% of infections. Vaccinated people won’t spread much disease. This has HUGE implications for developing guidance for fully vaccinated people and altering the trajectory of the pandemic.
Pfizer released new data from clinical trials showing that their vaccine protects for at least 6 months. Protection will likely be longer – so far we only have 6 months of data – and only time will tell how long. Studies have also found that these vaccines work well against at least some variants, and are highly effective against the B.1.351 variant first identified in South Africa.
Getting vaccines in arms
Now we have to get vaccines into arms around the world. Transfer of mRNA technology is key, because this technology can be tweaked for variants and is less susceptible to production problems. A biological vaccine process made into a chemical, more predictable one.
There’s no question that the vaccines are working. Look at the striking impact protecting the elderly in Michigan. Vaccines rock… but, we’re failing to get them to where they are most needed.
Israel is crushing the curve with vaccines. But more places need more vaccine – and quickly – especially Brazil and other places that are being hit hard.
Despite glitches (see: J&J/Emergent’s 15 million botched doses), supply keeps increasing. The US is vaccinating more than 2.5 million people a day now. BUT: the quality of vaccination – getting vaccines to those at highest risk – is important, and probably more important right now than quantity. See why below.
Vaccine reluctance keeps decreasing. And more availability and more convenience will overcome much of the remaining reluctance. A new survey from Kaiser Family Foundation shows that the “wait and sees” are deciding to get vaccinated – but that the proportion of “reluctants” is holding steady.
Variants going wild
The news on variants is mixed, but mostly bad. On a positive note, Israel’s success shows that these vaccines beat these variants. But many new variants are spreading rapidly in the US.
Deaths aren’t falling nationally as rapidly as I had anticipated they would – likely because the variants are not only more transmissible but also more lethal. @EricTopol summarized the data on variant lethality well.
Some think SARS-CoV-2 may be running out of genetic tricks and won’t be able to evade vaccine-induced immunity, and I hope they’re right, but hope is not a plan. We have to anticipate the possibility of vaccine escape mutants and reduce uncontrolled spread wherever it occurs.
Vaccine equity is imperative
Now the most important point of this article and the reason I wrote it this week after planning not to write one. Equity, equity, equity. This is not just about what’s right ethically, but what’s essential for pandemic control in both the near- and long-term. Uncontrolled spread anywhere is a risk everywhere in the long-term because of the possibility that even more dangerous variants will emerge. But that’s not the only problem with the current unequal distribution of vaccine.
If we just chase the number vaccinated, we miss the point. Equitable vaccine distribution will lead to maximum impact from vaccines – for fairness, to reduce deaths, to reduce cases, and to reduce risk of emergence of even more dangerous variants.
100 million people in the US have received at least one dose of vaccine. But about 50 million people over age 50 (~37M age 50-64 and ~13M age 60+) haven't been vaccinated at all. Vaccinating these people, who are disproportionately Black and Latinx, will prevent many more deaths than vaccinating young people.
Think of it this way. Targeting vaccinations to people at highest medical risk – who are 10 to 100 times more likely to die if they get infected – is 10 to 100 times more likely to save a life. We'd have to vaccinate 10 million people at low medical risk to save as many lives as vaccinating 100,000 to 1 million people at high medical risk.
And targeting vaccinations to the communities at highest risk for spread is MUCH more likely to prevent cases than targeting vaccinations where there is low risk of spread. In some low-risk communities, 0.6% of the population may be infected each month, while in high-risk communities, it may be 6%. With a vaccine that offers 90% protection, if we vaccinate 1M people in low-risk communities, 5,400 cases would be prevented. In contrast, If we vaccinate 1M in high-risk communities, this would prevent 54,000 cases – 10 times as many. This difference will compound in future generations of spread, so the actual impact could be 40 times to even 100 times larger.
In other words, a single well-targeted vaccination could save 10 times more lives, and prevent 100 times more cases, than vaccinating a low-risk person in a low-risk community. This is the essential fact we must act on. Equity isn’t only good ethics. It’s essential for epidemic control.
“The availability of good medical care tends to vary inversely with the need for it in the population served.”
— Dr. Julian Tudor Hart, in The Lancet (1971)
###
An Epidemic of Vaccine Inequity – March 29, 2021. Last Weekly Analysis.
As predicted, a 4th surge of Covid appears to be beginning in the US, fueled by spread of variants and by premature reopening. As CDC reports in its Covid Data Tracker, cases are up 7% nationally, and the test positivity rate is also inching up, now at 4.7%. Because the pace of vaccination has been accelerating, my prediction is that despite a 4th surge, deaths won't increase substantially. But we must solve systemic issues of vaccine inequity, both in the United States and globally.
One particularly concerning trend is in Michigan. Hospitalizations in Michigan are increasing rapidly, especially among 40-49 year olds. There is a 30% increase in cases at middle and high schools associated with new outbreaks, in tandem with increased community transmission. Fewer people are staying home, a rate that is now similar to pre-pandemic levels. Is this a harbinger of spring surges elsewhere?
Vaccines are getting into arms
Vaccinations are continuing at a high rate: 2-2.5 million per day. That’s about 1% of eligible Americans every day – the challenge isn’t to increase much more but to keep up that pace to meet the new goal of 200 million doses of vaccine administered by the beginning of May. And, even more importantly, to improve targeting. Expanding eligibility helps. Increasing availability of the J&J vaccine helps. And communication about expanded eligibility, how to schedule appointments, and where to get vaccinated helps.
It’s essential that we fix the horrific inequities in vaccine administration. Scarcity is the enemy of equity. North Carolina and Chicago have succeeded in providing vaccination that is roughly equivalent to the population breakdown, but nearly everywhere else – at least where I’ve seen the data – is only reaching Black and Latinx people at about half the rate of White people (Asian and Native American/American Indian access is variable, depending on the population – see re Navajo Nation below as one example).
This is even worse than it sounds, because Black and Latinx people are much more likely to get Covid and to die from it. In effect, other than the long-term care program (see below), we are aiming our shots in a way that doesn’t do nearly as much good as it could..
It’s not enough to be concerned about equity, and it’s not enough to have programs that attempt to address it. We must succeed. Vaccinating specifically in hard-hit communities, with J&J vaccine in addition to Moderna and Pfizer, is one important approach that needs to be scaled up, and fast.
Vaccines are saving lives already, and will save even more in the coming months. As I estimated last week, at least 40,000 more people would have died in US nursing homes and elsewhere since the beginning of 2021 without vaccines. Credit where credit due: the Long-Term Care vaccine program is a big success!
And as reported in NEJM, there was a marked decline in SARS-CoV-2 infections among health care workers at a medical center in Jerusalem after a vaccination program was initiated there. Another example of vaccinations working!
3 big gaps in the US vaccination program
1. Equity. Black and Latinx people are still about twice as likely to be killed by Covid but only half as likely to be vaccinated. We mocked up a data visualization (DATA NOTE REAL!) to show how metrics could be reported. Every place should publish something like this to track their progress as they implement programs to fix inequities.
2. Doctors. Covid vaccination should be available in just about every doctor’s office, in addition to pharmacies and community vaccination sites. Many people who are reluctant to get vaccinated elsewhere will get vaccinated by their doctor. We need all hands on deck to end the pandemic.
3. Convenience. Polls show that many people who want to be vaccinated haven’t been able to get vaccinated. Variability among states – and even within states – is big. Particularly as the J&J vaccine becomes more available, 1-shot vaccination at malls and other sites will be important. Convenience trumps reluctance.
Two questions about vaccines
First: How strong and long-lasting is vaccine-induced immunity? It looks very strong, but duration will take time to determine. And there will undoubtedly be some vaccine failures – people who get sick after being fully vaccinated. Such failures have been amazingly rare so far, and, when they have occurred, illness has been mild.
Second: Will variants evade vaccine protection?
We need to continue reducing uncontrolled spread wherever it occurs, for ethical as well as epidemiologic reasons. The risk of dangerous variants is proportional to the amount of uncontrolled spread.
Vaccine side effects are rare
We also need to look closely at the data about the AstraZeneca vaccine and possible increased risk of blood clots. No vaccine is 100% effective or 100% safe, and some people will experience adverse events after vaccination. The challenge will be to determine if those events are caused by the vaccine, or are just coincidence.
As reported in BMJ, after 20 million doses of the AZ vaccine have been administered, less than 40 blood clot cases have been reported. Is there a link? Maybe, but even if so, it is not strong – and the benefits of vaccination still far outweigh risks. We need to resist drawing causal links where none may exist.
We’ll find out about vaccine failure when there are breakthrough cases, and about very rare adverse effects, if there are any, when many millions of people are vaccinated. So far, the vaccines are astonishingly safe and effective.
Navajo Nation success story
One great success story about the effectiveness of vaccines and a public health approach: the Navajo Nation has crushed the curve. Their impressive vaccination campaign has resulted in 57% receiving at least 1 dose (compared to 26% of the US population). They also maintained a mask mandate and continue to provide free masks and hand sanitizer and discourage travel. The result: cases and deaths have gone down to zero.
Global Vaccine Inequity
Global vaccine inequity is horrific. There is simply no ethical justification for healthy young people in any country getting the vaccine before seniors or health workers in any place where the virus is spreading. We must rapidly increase vaccine production and distribution to all countries, regardless of income level.
Although the vectored vaccines are less expensive, easier to store, and are single-dose, mRNA technology has a lower risk of missing production targets, is more adaptable to variants, and faster to scale. Basically, mRNA technology is as close as an insurance policy as we can have against production delays and variant vaccine escape. But we must scale up production of vaccines that are proven, with publicly available data, to be safe and effective.
Vaccine nationalism is ethically inexcusable but politically inevitable. Inevitable unless, of course, you’re Norway. Again showing moral and financial global leadership. Norway played a critical role in the development of many global health initiatives, and may well help create a better global system of solidarity and safety.
Cases are increasing again in many countries. Brazil, Kenya, Ethiopia, Poland, and the Philippines are just some of the countries struggling to control transmission and treat patients. We need control measures and vaccines quickly, for everyone. Until all are safe, we are all at risk.
Covid and mental health
The MMWR reports important new data on the mental health harms of the pandemic in the US, with at least 12 million more Americans struggling. There have been large increases reported in depression and anxiety, especially among young people and those with lower levels of education. Availability of treatment hasn’t kept up.
Lab creation unlikely
It’s very unlikely that SARS-CoV-2 was created in a lab. The genetic information strongly suggests that the virus evolved naturally. Is unintentional lab release a possibility? Yes, as the review commission has noted. In many ways, what happened doesn’t change what we need to do going forward. Whatever happened, we need better global lab safety and security.
The last smallpox case in the world was from a lab error in the UK. A flu strain accidentally released in the former Soviet Union in the 1970s may have spread around the world. Let’s work together globally to make laboratories safer and reduce the risk of future health threats.
Two great unknowns
First, what will humans do. Will we lose motivation to continue our fight against the virus as vaccines roll out? Will we fail to maintain patience, discipline, and solidarity?
Second, what will the virus do. Will variants evade the vaccine?
The future isn’t certain, but it’s certain our actions can make it safer.
Not goodbye, but au revoir
After 14 months writing weekly on developments in Covid epidemiology every Friday night, I’m stopping. I may launch a weekly analysis including Covid to other public health issues. Remember, the right answer to epidemiologic questions is often: It depends. Life is complex, wonderful, and evolving. Thank you for reading!
It’s been said the only thing certain in life is death and taxes. To that, we must add the threat of future pandemics.
Covid is far from over, and the next pandemic could start any time. We must be better prepared, healthier, and more coordinated globally. Our public health and primary care systems need long-term investment.
Microbes outnumber us. If we work together, we can outsmart them.
“Encountering apathy, ignorance, and avarice is the lot of all conscientious health officers. As preventive measures in the health area are more successful, the public is less inclined to support the programs which ensure this success.”
— John Duffy ###
Progress and Peril – 3.22.21
Vaccinations have already saved 40,000+ lives in the US, and the pace keeps increasing. But explosive spread of variants in Brazil and lower interest in vaccination are ominous portents.
A 4th surge is likely in the US, but most likely a less deadly one than before.
Epi tells the story
First, the epidemiology. Cases are trending down, but have stopped decreasing in many places, and are increasing in some areas. New cases are plateauing nationally at about 50,000 per day, as reported by the CDC Covid Data Tracker (shown below), as are test positivity rates, with a concerning trend of PCR test positivity increasing slightly to 4.3% last week. Vaccinations are preventing deaths
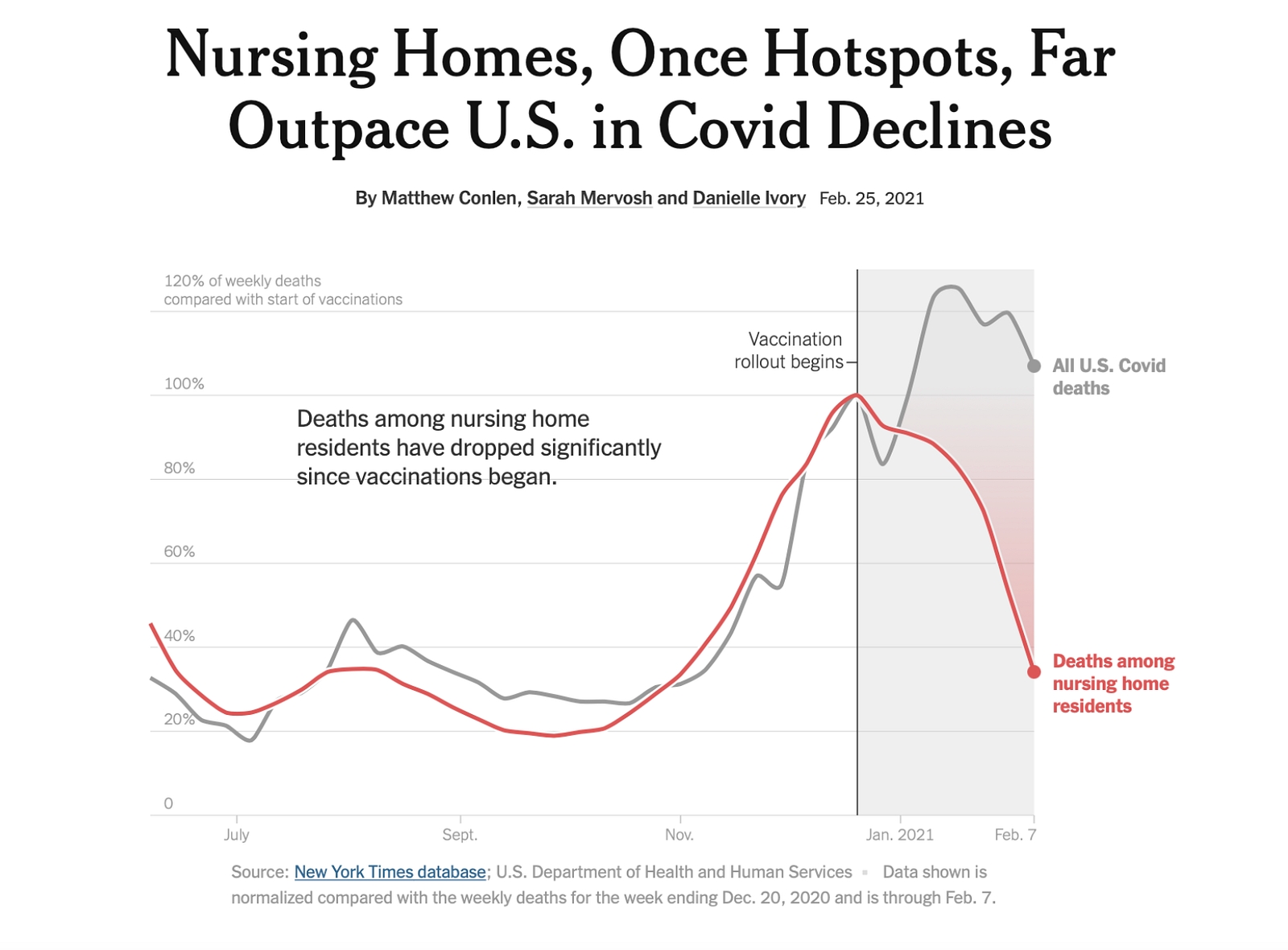
The faster decline in deaths is striking and undoubtedly due to vaccination. Look how steep the decline in the red line is in the graph below. Because vaccination rates in people over 65 are so high, especially those in nursing homes, the lethality of the virus is decreasing – and that’s a result of vaccination.
We estimate that vaccines have likely saved at least 40,000 lives in the U.S. Here’s a simple way to calculate that. Previously, about 40% of reported Covid deaths were among nursing home residents vs. about 19% of the roughly 200,000 deaths in 2021 so far. If nursing home residents still accounted for 40% of Covid deaths, 40,000 more people would have died since January. That may be a slight overestimate for nursing homes, but when you other vaccinated people whose lives the vaccine has saved, the number would be much larger.
Expect a 4th Surge
Will we have a 4th surge? I think so, but it won’t be as huge and not nearly as deadly as past surges, because so many of the most vulnerable people have now been vaccinated. The more we mask up and distance, the less we travel, and the faster we vaccinate, the fewer cases, hospitalizations, and deaths there will be.
Although winding down, the Covid Tracking Project is still providing important information. The trends in Michigan are concerning – with cases and hospitalizations increasing.
Cases are increasing in parts of Europe, often despite masks and distancing, following vacation travel. Travel is an accelerator of viral transmission. Traveling over spring break – while the virus isn’t taking a break – is not a good idea.
Vaccines are increasingly available – for some
As reported in @CDCMMWR, there has been surprisingly high second-dose vaccine completion – largely among the long-term care population and health care workers. We should expect this proportion to decrease as more groups get vaccinated. The single-dose J&J vaccine will be a big help in many settings (shopping center vaccination, anyone?).
You shouldn’t have to live in the right place or know the right people to access vaccines. @NYTimes highlights inequities in vaccine distribution; 43 countries, nearly all of them high-income, are on track to vaccinate all or most of their populations in 2021, but 148 are not. Ramping up mRNA production is a promising approach to getting more shots on arms.
In the US, it will be increasingly difficult to keep up the pace of vaccination. Many of the most eager got vaccinated right away. Next will be the willing, then the reluctant, and finally the late converts. For each area and demographic, the key will be to listen and address concerns with right messages – and the right messengers. Last week I participated in a fascinating focus group on this. Guess what Trump voters wanted to hear most? Being respected and listened to and having their factual questions answered honestly and forthrightly. Exactly what every group deserves and needs.
Variants are the wild card
Brazil presents a cautionary tale. Uncontrolled spread and slow vaccination rollout led to a huge wave, even though there had already been a devastating earlier wave. It seems likely that the P1 variant can reinfect people, although evidence for this is still emerging.
The B117 variant is spreading throughout the US, and may be associated with higher risk of death. Growing evidence suggests that available vaccines protect against this variant, according to a preprint article by Oxford University researchers, but the bigger problem is the possibility of newer variants. Immunity after infection isn’t perfect, and immunity after vaccination may be able to be overwhelmed by variants that haven’t yet emerged.
Those who have had COVID-19 should still be vaccinated! An interesting study from Denmark published online by @TheLancet suggests that previous infection provides 80% protection against reinfection, but that protection among those age 65 and older was only 47%.
More people getting vaccinated means that selective pressure on the virus will increase, and if strains emerge that can evade this immunity, these strains can spread. We don’t know if this will happen, but we know it’s a risk, and we know that we can reduce that risk by reducing uncontrolled spread wherever it occurs and increasing the pace of vaccination.
Inching toward the new normal
The virus is a wily enemy, and @HelenBranswell highlights an investigation published in @CDC_EIDjournal that demonstrates just how contagious it can be. If we let our guard down too early, Covid will take advantage.
With protections in place, especially masks, we can begin to do more as vaccination makes the virus less lethal – and adjusting our response if cases start to rise. The virus has had a major impact on many facets of our lives, from schools to jobs, and recovery will take a while.
Multiple studies demonstrate that schools can open without excess Covid risk, and @CDCgov has appropriately updated its guidance. However, the more Covid spreads in a community, the higher the risk for everyone, including school staff and students.
Covid is reversing health progress
In some places, the pandemic's impact hahttps://app.gitbook.com/@simpledotorg/s/tf-articles/~/drafts/-MWKrBmuVOAxArHGUg7b/tom-frieden-blog#variants-are-the-wild-cards been as harmful as Covid itself. Data from 19 @_AfricanUnion Member States, reported by the Partnership for Evidence-Based Response to COVID-19 (PERC), shows the extent that the pandemic has driven food insecurity and disruptions to health services. We must increase equitable access to vaccines.
A new report from @StopTB shows that Covid set us back years in TB control. As many as a million patients may have been missed as a result of the lack of access to health facilities. Each one can potentially infect other people. This is a truly devastating setback.
As reported in @Nature, this timeline of progress from the past year is remarkable. Scientists across the globe made rapid progress against the most disruptive health threat of the past century – but there is so much more we need to learn!
“We ignore public understanding of science at our peril.”
— Eugenie Clark
###
It Ain't Over 'Til It's Over -3/13/21
The U.S. has now hit two milestones in the Covid pandemic: 100 million total Covid infections in the US (most of them undiagnosed), and as reported by the CDC, 100 million vaccine doses administered.
In the race of vaccination vs. variants, we're gaining on the virus. It’s slow progress that we hope to accelerate as more people get vaccinated. But nobody should declare victory in the third quarter. Safer doesn't mean safe.
Encouraging progress
@CDCgov reports encouraging progress in its weekly Covid summary and website, both of which continue to get better:
11% decrease in cases this week;
Test positivity rate is down by 11%, to an encouragingly low 4.1%;
Vaccinations up to 2.2 million per day, an 8% increase over the prior week;
65 million people have received at least one vaccine dose and 35 million are fully vaccinated;
Deaths are down 19% – this decrease is faster than the case decrease, and represents thousands of lives saved by vaccination.
But better doesn’t mean good. Rates are lower, but they’re still still very high:
More than 50,000 new cases a day;
Nearly 5,000 hospitalizations last week;
More than 1,400 deaths a day.
Variants remain concerning
Right now we’re in a race between vaccination and variants. Which of them wins will determine whether there’s a 4th surge. Variants are spreading, and may now be responsible for more than half of NYC Covid cases and a growing proportion elsewhere.
Think of the most concerning variants as the “B1 bombers”: the B.1.1.7 variant, first identified in the UK, which is more infectious and likely more deadly, and which is doubling in the US every 10 days; the B.1.351 variant, which emerged in South Africa and reduces the effectiveness of some vaccines; and the B.1.526 variant, which is spreading rapidly in NYC. All of these variants increase the risk that the virus will overcome immunity from natural infection.
Fortunately, per @NEJM: The Pfizer-BioNTech vaccine appears to overcome the P.1 variant first identified in Brazil, another of the more concerning variants. But that’s no guarantee new variants won’t escape vaccine-induced immunity. The more the virus spreads, the greater the risk.
Is a 4th surge looming?
Will there be a 4th surge in the US? Those who answered this (admittedly unscientific) poll are optimistic there won’t be.
How well variants do depends partly on the virus, but mostly depends on us. That’s why it’s critical that we continue to wear masks, maintain distancing, and vaccinate quickly. It’s a mistake to lift mask mandates while the virus is still spreading at dangerous levels throughout most of the country.
And, as reported in BMJ this week, the variants may well be more deadly. Now that we can see that there may be an end in sight, we don’t want to let down our guard too soon. The pandemic isn’t over. Not in the US, and certainly not globally.
People who have been vaccinated aren't out of the woods. We can’t assume that the vaccine has kicked in to provide sufficient protection until 2 weeks after full vaccination.
Getting vaccines into arms
The CDC has issued guidance on what people who have been fully vaccinated can safely do – and what they should not. This guidance, with the science brief that supports it, is a good example of evidence-based recommendations. As noted in this week’s JAMA, we need to have a clear discussion of what this guidance means for people day-to-day. As more data become available and more people get vaccinated, these recommendations will evolve. That’s how science works.
No vaccine is 100% effective. And every vaccine has some rate of adverse reactions – but the risks from vaccines are much less than the risks from infection.
Scaling up vaccination requires using multiple platforms: mass vaccination sites, networks of doctors’ offices and pharmacies, pop-up locations – even mobile vaccination clinics to go door-to-door in hard-hit and hard-to-reach communities.
Soon we will go from having too few vaccines to having too few arms to put vaccines into.
We need to continue to find and address barriers to vaccination: to access, to understanding, and to acceptance. And as a recent poll indicates, there are wide gaps in people’s willingness to get vaccinated.
Re-opening
We should open schools and businesses safely. However, restaurants, bars, and large indoor events are much riskier, especially in places without mask mandates. A new MMWR study shows that masks work, and that places allowing on-premises restaurant dining had higher case and death rates. No worker should be avoidably exposed to Covid, or have to plead with a customer to mask up. OSHA should act.
Approximately 1 of every 200 infections in the US results in death, and therefore, with more than 500,000 deaths, there have been more than 100 million people infected already. (The 100 million estimate is also consistent with serological studies and epidemiologic models suggesting that 25-30% of Americans have been infected.) Globally, with a younger population, there may be one death per 300 or more infections – but we also know that Covid deaths are under-reported. There may have already been a billion Covid infections globally.
Five points to end the week
First: Covid is far from over. Have a look at the map from @NYTimes below. It’s still raining Covid pretty hard out there.
Second: Think about the next generation and how they will be affected by the pandemic in the long term. This cohort was to have been dubbed Gen Alpha, but now maybe they'll be Gen C (for Covid), skipping A and B after Generations X, Y, and Z.
Third: We need to recognize the failures at local, state, national, and global levels. No institution got it right. U.S. public health systems had pre-existing conditions that increased our vulnerability. We need long-term solutions.
The Trust for America’s Health just released a good report: Ready or Not? Sadly, the verdict right now is NOT. We can change that. We need to improve emergency response, public health, and primary care. In an article in AJPH, I’ve outlined what’s needed broadly and on cardiovascular health. Even BEFORE Covid, US life expectancy was lagging behind other countries’ – more disability, more illness, earlier death.
Fourth: We must build health resilience against Covid and other health threats, including the leading preventable killers. The Biden-Harris Administration can build on success stopping Covid. Start with preventing heart attacks and strokes, which will kill nearly a million Americans this year. As we explain in an article just published in JAMA, most of those deaths can be prevented.
And fifth: Stay safe. Keep masking up. Remember the mantra: patience, discipline, solidarity. The sooner we get to the new normal, the better we will all do.
“It ain’t over ‘till it’s over.”
— Yogi Berra, Great American Philosopher (and Catcher)
###
Keep your mask and guard up!
Are we finally nearing the new normal? By May we'll be much safer – but we're not there yet. Vaccine rollout continues to gain momentum, saving lives. Cases are still trending down, although the declines are slowing. But transmission is still high in most of the country, and variants could quickly derail the progress we’ve made. Hang in there!
Farewell Covid Tracking Project
A HUGE thank you to all who worked on the Covid Tracking Project, which wound down this week. Their final weekly metrics are reported in the graphs below – this comprehensive level of data collection and analysis has not quite been replicated by @CDCGov, but the CDC’s weekly Covid Data Tracker is getting there. The blip in case decrease last week seems to have been mostly weather-related, with cases still trending down, but we’re not out of the woods.
Bookmark this for future reference (I did): Where to find and how to use Covid data. As impressive and helpful as this effort was, I hope we never again need something like this – that the Federal government never again abdicates its responsibilities.
Look at the orange line in the graph below of new cases. I’ve drawn in a heavier black line to highlight the dip, which is most likely due to both the effects of bad winter weather throughout much of the country (less testing leads to less diagnosis) and an actual slowing in the rate of the decline. The rate of decline is slowing (note that the slope of the black line is less acute than that of the orange line). This may be because there are more exposures and increased spread of variants.
Deaths down, risks remain
Now some REALLY good news. As I’ve predicted for the past few months, we’re seeing a rapidly decreasing case fatality ratio with an even more remarkable decrease in nursing home deaths. This is the direct impact of vaccination: It saves lives. Within a month or less, the number of deaths should decline to less than 1000 a day. This is still horribly high, but much lower than it’s been for many months.
For some perspective: Nationally, there are more than 50,000 cases diagnosed per day, or about 15 new diagnosed cases daily per 100,000 population. This translates to about 1 in 6500 people in the US diagnosed every day. (Remember, too, that only a fraction of cases are ever diagnosed, and that infected but undiagnosed people can still spread the virus.)
People are infectious for roughly 7 days (possibly 10 with some of the variants). So let’s assume that about 1 in every 1000 people is infectious at any given time. If only one in 2-3 infections is diagnosed, it’s more like 1 in 400 people. In a month, if you have contact with 100 people (and some people in frontline positions have many more than that), there’s a 1 in 4 chance of being exposed. That’s not small.
Complacency = Death
It’s still raining Covid pretty hard out there. There’s now twice as much testing than there was in September, with similar case counts, so there’s been real progress. But, as an example, there are still more than 3,000 new diagnosed cases a day in New York City, at least 10 times more than outbreak investigation and control can realistically manage. And with the increased danger posed by more infectious variants, we’ll need all the tools at our disposal to prevent yet another wave of widespread disease transmission.
By next week, we’ll hit the milestone of 100 million total infections in the United States and, possibly, as many as 1 billion globally. Stay tuned – I’ll discuss these estimates and the basis for them in my blog next week.
The more contagious P.1 variant, first identified in Brazil, is concerning. So is the increased spread in children (but with no increase in severe illness), although this doesn’t change what should be a policy priority: To open schools and keep them open with proper mitigation strategies. More infectious variants will become much more prevalent in the US, but if we’re careful, they won’t drive a 4th surge.
Vaccines work, but keep masking
On vaccines, the theme of the week is MORE. More good news. More people getting vaccinated. More vaccine options. And soon, much more vaccine access. Once you’re vaccinated, there are a lot of things that you can do with relative safety. Get a haircut, see the dentist, ride the subway, hug your grandkids, take that long-delayed vacation.
But don’t assume that vaccines provide perfect protection, and continue to mask up. If you’re older, remain cautious about gatherings with people outside your immediate household. If you develop any Covid symptoms, get tested as soon as possible.
Interestingly, CDC data suggests that the vast majority of people who got the first dose of vaccine are returning to get the second dose. This is encouraging and a pleasant surprise.
Vaccines are astonishingly effective, safe, and increasingly available – at least in the US and some other wealthy countries. But persistent national and global vaccine inequities are unethical and dangerous, and the US is in a unique position to fix this problem.
There are many routes to vaccine efficacy. Some interesting data shows that vectored vaccines (J&J, AZ/Oxford, Sputnik) may provide stronger immunity after 1-2 months. How long immunity lasts from single-dose vaccines has yet to be determined. And although we have highly effective vaccines from which to choose, there is still much, much more we need to learn about them.
Stop the madness about mask mandates
How do you solve a Governor like Abbott? (And others. Many others.) If OSHA can enforce worker safety standards for private business – many of which are support mask mandates – businesses might ask governors to do the right thing and enact (or at the very least not pre-empt) mask mandates.
There’s some great new CDC data on how facemasks reduce Covid cases and deaths. Simply put: Science saves lives. Great to see CDC back in the game.
Cool it just a little bit, public health. Reopening – while still managing to avoid superspreader events – as cases fall and vaccines make Covid much less deadly may be wrong, but may be defensible. However, relaxing mask mandates is NOT defensible. The only freedom masks inhibit is freedom of the virus to spread and kill people.
After Florida repealed its motorcycle helmet law back in 2000, helmet use dropped from nearly 100% to about half. This reduction in helmet compliance was at least partially responsible for a sharp increase in motorcycle fatalities. Costs of emergency medical care for motorcyclists hospitalized with head, brain, skull injuries more than doubled, from $21 to $50 million. Mandates work. Reversing mandates reverses progress.
Adapting to a new normal
Covid may never go away completely, but we can minimize its dangers. What will change as we tame Covid? Less travel. Fewer meetings and conferences. More (but less than now) Zoom. We may never see birthday candles in the same way. The virus adapts. Unless we adapt, it will continue to control us. The more we adapt, the more we can control it. Masks help, and will also help control seasonal influenza. I don’t know of anyone who wants to get the flu.
“Throwing out preclearance [mask mandates] when it has worked and is continuing to work to stop discriminatory changes [infections and death] is like throwing away your umbrella in a rainstorm because you are not getting wet.”
— The Notorious RBG ###
The End is Near! But Not for the World
There is now steady good news about Covid in the United States. Cases, hospitalizations, and deaths continue to decrease, and the pace of vaccination is accelerating. Serious risks remain from variants, vaccine inequity, and failure to learn the lessons of Covid.

First the good news. As reported by the CDC, US cases have decreased 75% from their peak in early January, with hospitalizations and deaths following. Vaccination (after a weather-related disruption) is increasing, and much more supply is on the way — the Johnson & Johnson vaccine will add millions of doses ready to the supply. If things continue to go as planned, by June anyone in the US over age 16 who wants a vaccine should be able to get one.

Vaccinations are saving lives
As reported by The New York Times, there has already been tremendous progress driving down Covid deaths in nursing homes, which has happened more rapidly than in the US as a whole. As I’ve been predicting for the past two months, we can expect even larger reductions in deaths in March as vaccine-induced immunity kicks in. The risk of death from Covid among all those infected will fall by at least two thirds.
Covid tamed?
Will vaccination make Covid no deadlier than seasonal influenza? There are at least two major problems with that question: First, with high infectivity and moderate case fatality, Covid would at best still be like a moderately severe flu. And, flu is the Rodney Dangerfield of infectious diseases — it doesn’t get the respect it deserves.

Every year in the US, flu causes tens of thousands of deaths, hundreds of thousands of hospitalizations, and billions of dollars in health care and economic costs — much of which could be prevented. Flu vaccination works, but not very well, and not as well as Covid vaccines appear to. Masks and distancing crush the flu curve, although it’s not something we’ve regularly done in the US as in other countries. Maybe we should start.
Variants are the wild card
Now, the bad news. The worst news of the past month is that data from the Novavax trial in South Africa suggests that prior infection might not prevent reinfection with the B1351 variant. But the validity of the antibody tests used in that trial is uncertain — so the jury is still out.
There’s been unnecessary controversy on variants. Attacks from all sides aren’t helping. The bottom line: Variants are DEFINITELY a risk and we also DEFINITELY don’t know how big a risk.
It’s better to be safe than sorry, but we in public health should also recognize that people (including politicians) may choose to take risks. But we hope they’re informed risks based on careful consideration of the data, community prevalence, and other factors grounded in science. Also, that we distinguish between risks we take where the risk is to ourselves and risks we take with others’ lives.
Think of it this way. It’s one thing to risk your life climbing a cliff. It’s quite another to do that when you might start an avalanche that kills people in the town below.
Why do variants spread? Sometimes they’re more fit and better able to reproduce. But sometimes it’s “stochastic” — a fancy word for happenstance. A superspreader event could be the starting point. Or it could be the founder effect. Or it might just be plain bad luck (or good luck, if you look at it from the virus’ standpoint). More common doesn’t necessarily mean more infectious or more dangerous.
Two puzzlers for the week
First: Why are US cases dropping SO fast?
See the arrows I’ve drawn in the second graph below from the Covid Tracking Project: US cases are dropping much faster in the most recent Surge 3 than they did in Surges 1 and 2. Was this because we started from a peak that was higher, which was driven by travel and holidays that are now over, increased masking up, and rapid roll-out of rational national policy? Maybe.

Imagine you’re a virus attacking 330 million people. 100 million have natural defenses from a prior attack. 10 million more are being vaccinated each week. The places where it’s still possible to land are shrinking. The concept of ‘herd immunity’ is another false dichotomy; the steeper slope of the current decline in cases is likely, at least in part, from increasing immunity.
(For those wondering about the 100 million number: That’s a reasonable estimate of the number of people infected in the US so far. There are various ways to estimate that. It’s simplest to estimate from the number of deaths to the number of infections at an approximate ratio of 1 to 200. So 500,000 deaths translates to about 100 million infections. Not all infections will result in immunity, and we still don’t know how long immunity will last.)
But the biggest driver of the decrease is us: masking, distancing, reducing travel. The odds of our experiencing a large fourth surge are falling steadily. But please, keep up your masks, your distance, and your perspective: 2,000 deaths a day is horrifying. A 75% reduction from a huge number is still a huge number. In a few more months, if all of us keep it up, we’ll be in much better shape.
Second: Why are cases in New York City not dropping nearly as fast?
I remain puzzled about NYC, which was hit hard and fast early in the pandemic. The decline there is real, but it’s much slower than the national decline. The baseline infection rate in NYC is higher, so it can’t be because of less immunity — there’s more. Test positivity rates are trending down, but only slowly as shown in the graph below, from NYC’s excellent site (which also shows 10-fold differences in risk in different neighborhoods of the city.) Variants are one theory (and a new variant has just been identified in NYC) but at this point it’s just that — a theory. Time will tell, for better or for worse, what is happening in NYC.

Vaccine equity
After variants, the second big risk is the lack of vaccine equity, both in the US and globally. Anywhere the virus spreads, more dangerous variants have a chance to emerge and threaten health everywhere. We need to scale up control measures, including vaccination, everywhere.
A safer future
The third big risk is that we fail to learn the lessons Covid has to teach us. We need new funds to improve preparedness ($5–10 billion or more a year, for at least a decade) and for strengthened primary care. WHO and other global institutions need to be stronger. There needs to be more technical collaboration, better management, and better immunization of public health from politics. In short, we need substantial changes in how we approach pandemic prevention and response.
And so much is still unknown about long-haul Covid. It takes many people a long time to improve, even from a relatively mild case of Covid. Some people have continued to suffer for many months with no end in sight. It’s important that NIH lead systematic studies so we can learn more and, more importantly, do more to help those who are struggling with persistent symptoms.
Not there yet
When will it be safe to go out again? This summer, the US will be much safer. Will we learn to cluster bust, stopping spread promptly even though Covid won’t be as lethal since the most vulnerable people will have been vaccinated? Will variants evade our defenses? And will we help the world stop Covid?
Answers to these three questions will determine how much normality we get back and how soon. Often in public health, the right answer to a hard question is: “It depends.” In this case, it depends on us. Can we strengthen test/trace/isolate strategies to box in the virus as its potential landing places continue to shrink? Can we scale up vaccine manufacturing and distribution for the entire world?
Last week, the US reported 2,000 deaths per day. PER DAY! For the past 3 months, as shown in the graph below, Covid has killed more people in rich countries than the leading cause of death: cardiovascular disease. At Resolve to Save Lives, CVD is a primary focus. (Link in sentence above is from an excellent website visualizing the pandemic and its inequalities.)

This past week marked exactly a year since it became clear that a pandemic was inevitable. I summarized some of our work this past year in CVD and other areas in a message to our partners. To see more about what Resolve works on and where, here’s a link.
Covid isn’t over. Right now we have no idea what the upticks below (as reported by Our World in Data) mean and whether they will persist. Again, time will tell. We need to keep our perspective. A lot better still doesn’t mean good. Covid remains rampant. Global control is essential.

“Not everything that is faced can be changed; but nothing can be changed until it is faced.”
— James Baldwin
###
Safer Doesn’t Mean Safe (Yet)
2-20-21
Covid cases continue to plummet, although a small part the recent decrease may be due to weather-related testing site closures. And while vaccination roll-out is going more smoothly, we must address equity much more effectively. Deaths are decreasing. Global collaboration is rising. Spring, not Covid, is increasingly in the air.
Better, But Not Yet Good
Covid decreases are steep, sustained, and nation-wide. Cases decrease first, then hospitalizations, then deaths. There are four major reasons for the decrease: less travel, less mixing of people indoors, more consistent mask wearing, and growing immunity from infections (about 30% of the US population) and vaccination (12% have received at least one dose). Herd immunity isn’t an on-off switch; increased population immunity – primarily from infection, not vaccination – is likely accelerating the decreases. The virus has less and less room to maneuver.
But herd immunity also isn’t uniform across society, and most people are still susceptible.
Better does not mean good, and safer does not mean safe. More than half of the American people are still susceptible to becoming infected, and infection rates remain quite high in many places. We’re still higher on all three metrics – cases, hospitalizations, and deaths – than we were in September and October when the current, now subsiding wave started to pick up steam. So, although the situation is much improved over the past month, we’re still not where we were at the end of summer.

Ongoing surveys by Carnegie Mellon University using the Facebook platform show that we’ve sustained our behavioral change surrounding Covid. Changes in mobility and mixing were the major drivers of both the recent increase and the current decline.
The bumps over the winter holidays boosted and accelerated viral spread, and the tide is now steadily ebbing. But continued declines are not inevitable. We have to keep up our guard, or the virus, armed with new variant tools, could come roaring back in a deadly 4th wave.


Variants Are the Wild Card
Variants continue to be THE wild card in controlling the pandemic. If mutations mean the virus is better able to evade natural or vaccine defenses, the risk of explosive spread is high. CDC’s excellent weekly Covid summary notes that we can “stop variants by stopping the spread.” The overall national test positivity rate is down to 5.9% (although it’s double that or more in some parts of the country), but last week there were, in shocking numbers that we have become too accustomed to, 7,000 new hospitalizations and 2,700 deaths every day.
Another great thread by @youyanggu points out that a doubling every 10 days of the B.1.1.7 variant as a proportion of all Covid cases doesn’t mean a doubling in total B.1.1.7 numbers. More detailed projections about the impact of this variant have been published in the MMWR. The graph below from a preprint article may explain at least some of the increased infectivity of the B.1.1.7 variant, which may be due to a longer period of infectiousness.

Death and Vaxes
Although vaccination has not yet had a major effect on Covid cases overall, it IS driving down nursing home deaths: the share of deaths associated with long-term care facilities has been cut in HALF since early January, from more than 30% as a proportion of all deaths from Covid to less than 20%.
With most nursing home residents and many other people over age 65 having been vaccinated, I will make a prediction: the infection fatality ratio will likely drop from the current 1 in 200 infections resulting in death to less than 1 in 600 by some time in March.

There’s a good article in @NEJM about effective communication strategies that can be used to encourage the “moveable middle” of vaccine-hesitant people to accept vaccination. But convenience overcomes reluctance – and the continued difficulty that many BIPOC individuals experience in accessing vaccines perpetuates the unjust, racist power dynamics of the US.
Let’s talk about death – uncomfortable as it is, we need to do that more. We also need to highlight the harsh inequities of Covid. There were 344,854 reported Covid deaths in the US in 2020, of which 37% occurred in the first half of the year. CDC just published a new Vital Statistics Rapid Release with data showing the projected life expectancy decreases driven by these deaths.
Americans as a whole lost a full year of expected life due to Covid, but this jumps to 1.9 years lost for Hispanic people and 2.7 years for Black people. These decreases erased many years of health progress in just a few months.
Before we do a deep dive into the numbers, let’s try to never forget that each one is an individual whose life was tragically lost earlier than it otherwise should have. A deeply moving effort by @washingtonpostattempts to provide some sense of the enormity of our losses. Please read it.

Since more than 60% of US Covid deaths took place in the second half of 2020, we can expect the actual decrease in life expectancy to be well over 2 years. The Black/White disparity may decrease slightly, but not because prevention and care improved for Black people in the US: As Covid accelerated its spread, the proportion of cases among Whites doubled.
There’s far too much missing data but the data is still stark – there are far higher rates of death among Black and Latinx people. Vaccination programs have to prioritize the hardest hit groups. Vaccine hesitancy is real, but lack of access is the driving reason for lower rates of vaccination among minority populations.

There’s new and troubling data from Zambia. Of 362 people in one study who died from any cause, 70 tested positive for Covid, but only 6 of those – less than 10% – were diagnosed before they died. How many Covid cases and deaths have we missed globally? Sometimes the dog not barking in the night is really no one listening. Improved reporting on causes of death is crucial to improve global health.
Vaccine inequity in the US is just a small microcosm of the vaccine inequity globally. The UN reports that 130 countries have yet to receive a single Covid vaccine dose.
Can we have a healthy arms race – to see which country can help other countries get the most vaccines into arms? Increased manufacturing will be essential if we are to meet our moral imperative to rapidly expand global vaccination availability.
Bill Foege notes that public health is at its best when we see, and help others see, the lives and the faces behind the numbers.
“We are only as blind as we want to be.”
— Maya Angelou
The Best of Times, The Worst of Times – 2.12.21
The third US COVID-19 surge is fading fast, but variants – some of which deeply ominous – are spreading fast. Vaccination is picking up steam, but we’re failing to address equity. And already high levels of pandemic fatigue are increasing. We must hang on for a few more months until most of us are vaccinated.

The fundamental question is whether we’ll have a 4th surge. If we do, it will cost lives, and also increase the risk that more dangerous variants will spread widely.
But first, some good news: there’s been a dramatically fast decline in cases and test positivity rates – a much steeper decline than in either prior surge. You can see it in both case counts, and test positivity – and test positivity is an even more revealing measurement, so the graph below, from Johns Hopkins, is the most encouraging graph I’ve seen in months.

The thing about wearing masks, not traveling, and minimizing time spent sharing indoor air with people who are not in our household?
They work. It’s how we can win the war against the virus. Any time we let down our defenses, it attacks. When we let down our guard (and masks), we are complicit with our viral enemy.
Calm before the variant storm?
The spike in cases which happened in other countries when variants took hold is scary. The proportion of cases from the B.1.1.7 variant (the “UK variant”) is now doubling in a bit over a week in the US, and may soon predominate here. The first known case caused by a COVID variant has also recently been found in a prison, where transmission rates are high.
This is no time for complacency – masks and distancing stop even the more transmissible strains.
As CDC put it in their weekly summary, which debuted today: “Better, but not good enough.” (It’s great to see the CDC able to share more of the important work and analysis they’ve been doing for the past year!)
Sign up for CDC’s weekly COVID Data Tracker newsletter. Hope that CDC adds the key metric of test positivity to their data next week.
Have a look at the @NYTimes graphic below, which our team at Resolve helped to design. It details county-by-county COVID risk. We’re doing way better than we were in December – but still way worse than in September.

And there are warning signs, including in NYC, where test positivity is not decreasing (as seen in the graphic below, from @NYChealthy). In the battle against Covid, a stalemate favors the virus. The next few weeks will be crucial: If we don’t maintain discipline, viral variants can cause explosive spread.

Variants very worrisome
But even more ominous is preliminary data from the Novavax trial in South Africa, with data, that, if confirmed would indicate that previous infection does not protect against reinfection with the variant strain. This would be the worst news about variants yet, because, if such variants spread, this would mean that prior infection would not count toward achieving herd immunity – a big setback.
Rates of infection, which was mostly with the 501Y.V2 variant (the variant first identified in South Africa) among the placebo group (those who did not receive the vaccine) 7 days after receiving the first placebo dose were 3.9% among those who tested seronegative, but exactly the same, 3.9% for those who were seropositive. If the serology was accurate, this suggests that prior infection didn’t protect people at all. This is quite different from other trials, in which seropositive participants who received placebo had protection rates of 80% or more, and studies in health care workers in the UK suggesting strong protection. Similar to breakthrough infections after vaccination, we don’t yet know if those infected despite immunity will have less severe disease, although we hope they will.
People born with severe immune deficiencies can harbor (and spread) the polio virus for years, and there has been work to identify, treat, and cure these people of their polio infection. Viral evolution and genetic recombination in immunosuppressed people is one theory for why we are seeing rapid genetic changes resulting in these SARS-CoV-2 variants. We need to learn, and do more to limit viral evolution and spread. One approach is to develop pan-corona vaccinations; good article on this by Dennis Burton and @EricTopol.
Vaccines remain in short supply
We are picking up the pace of COVID vaccination, and now averaging 1.6 million doses given a day. Both Pfizer and Moderna have promised to roughly double deliveries of their vaccines in next few weeks to meet President Biden’s goal of being able to vaccinate 300 million Americans by the end of summer. I hope the companies are able to keep that promise.
We must do MUCH better on equity. Black and Latinx Americans have 2-3x risk of hospitalization and death but only half the likelihood of being vaccinated. These continuing disparities are not acceptable and we need a concerted effort a national level and in every state, city, and community to empower and enlist communities and community leaders. Disproportionate burden means there must be disproportionately increased resources, including to find the right messages and messengers, and to make vaccination so easy that it becomes the default value. Convenience can overcome a lot of resistance.
The current math, unfortunately, is harsh. So far 70 million vaccine doses have been sent to states to be administered. We need 364 million doses for priority groups 1a (residents of nursing homes and other long-term care facilities, as well as health care personnel) and 1b (people age 75 and older as well as frontline essential workers), and those age 65-74 along with those who have underlying high-risk medical conditions (part of group 1c). And this would leave out people age 50-64 who are high risk, including those not aware of their underlying conditions. We’re looking at 1-2 more months of vaccine scarcity, at least.
Vaccination of nursing home residents and staff are likely to drive deaths in these facilities down by mid-March; this will also reduce the overall case fatality ratio significantly, since nursing homes account for nearly 40% of all deaths. Israel’s data is encouraging. A new preprint article published earlier this week shows the comparison between the population age 0-59 years old (orange line) and age 60+ (blue line) in new cases. Vaccination saves lives, and this is real-world proof of it, confirming the remarkable efficacy data from clinical trials.

Progress is possible
There’s good new CDC guidance on schools. Schools, especially grades K-8, should open with safety measures that emphasize consistent and correct mask wearing and maintaining proper distancing. Additional layers of COVID-19 prevention include testing whenever possible and vaccination as soon as possible. Teachers are – and should be – prioritized for being vaccinated. While we wish there was sufficient vaccine for everyone right now, including all teachers, unfortunately we don’t.
On Friday I published an article in the @WSJ (open access) on how to prevent the next pandemic. @ResolveTSLhas worked with partners on developing this strategy for the past 4 years. It’s now or never – a teachable moment like no other we’ve experienced in our lifetimes.
I suggest a global target: “7-1-7”. Every country and every community should be able to find an outbreak in 7 days, investigate and report in 1, and respond effectively in 7. Success will take money, technical skill, collaboration, and persistence. Our children’s safety depend on it.
Six steps to meet the 7-1-7 target are:
Agree on goals and how to measure them.
Build country preparation and response capacity, particularly with collaboration among lower-income countries.
Improve global institutions, with the World Health Organization as the anchor and a key role for The Global Fund.
Get money – at least an additional $5-10 billion a year to build country capacity to find, stop, and prevent health threats.
Collaborate to global response to address dangerous, life-threatening gaps in preparedness, including laboratory safety and reducing the risk of spread from animals to humans.
Act now – the urgency of this work has never been so clear, and there is no time to lose.
We need to hang in there. The pandemic won’t go on forever. We'll be in a much better situation by the fall. For now, mask up and limit time indoors with people not in your household. Vaccines are coming, and we learn more every day about Covid and how to prevent and treat it.
“No winter lasts forever; no spring skips its turn.”
Hal Borland, American author, journalist and naturalist
When day comes we step out of the shade,
aflame and unafraid,
the new dawn blooms as we free it.
For there is always light,
if only we're brave enough to see it.
If only we're brave enough to be it.
Amanda Gorman, US National Youth Poet Laureate from her Inaugural Poem, Jan 20, 2021
Don’t Ease Up on the Brakes! 2/5/21
Covid variants are here, and more are coming – but so are vaccines. There’s encouraging news: cases, hospitalizations, and percent test positivity are plummeting in all ages and in all parts of the country, and deaths have begun to decline.
Now the bad news: infections are still VERY high, and higher than at the peak of prior surges. The most likely explanation for the rapid rise and even more rapid fall: travel accelerates viral spread exponentially. We’re recovering from the huge amount of ill-advised travel and indoor contact over the holidays. When people travel, the virus travels.
This is a fight against the virus, but also a fight against becoming numb to the horrifying toll. Far too many who get sick are not recovering. The 7-day average is still 3,000 deaths per day, the number of people killed on 9/11. More than 20,000 died last week. Every life is precious. Every death robs us all.
As more people receive vaccines over the next several months, we can’t afford to ease up on the brakes now! Let’s double down on protection protocols (masks, distancing, limit travel), scale up equitable vaccine delivery, and spur innovation in vaccination and control measures. We can avoid another, steeper curve.
Vaccine Indicators
The sooner we vaccinate and the better we tamp down spread, the lower the risk from variants. We’ve had steady – though rocky and uneven – progress with vaccination. This week, @ResolveTSL and partners the American Public Health Association, Trust for America's Health, Association of Schools and Programs of Public Health, and Center for Health Security at The Hopkins Bloomberg School of Public Health released recommendations for vaccine indicators every state should collect and publicly share to inform decision-making and provide accountability and transparency in vaccine rollout.
There are two glaring gaps in the information the federal and state governments publish: data on vaccination by race/ethnicity over time, and vaccination coverage of staff and residents in nursing homes. Not coincidentally, there are problems not just with data availability but also with the reality in both areas. These are life and death problems.
First, race/ethnicity. We need to see vaccinations by race/ethnicity over time. Unless this is made available and updated weekly, there’s no way for us to know if we're getting better at addressing inequality or not. North Dakota is tracking vaccine coverage over time by age. We need the same data collected and reported over time on race/ethnicity, not just cumulatively.
Reports from the Kaiser Family Foundation show that data on vaccination by race/ethnicity is alarming. Ohio has a good Covid vaccination dashboard (see figures below)and, as appears to be case nationally, Black and Latinx people are getting vaccinated at about half the rate of White people, despite having 2-3x the death rate. We MUST do better.
There’s been great progress vaccinating nursing home residents, with about 80% receiving their first dose. However, the proportion of staff who have been vaccinated is under half. Because turnover of residents is high, including people moving between facilities, vaccination of people when they are admitted to nursing homes is essential and needs to be routine.
This will require implementing a model that’s different from the standard pharmacy program for Covid vaccination. Unless there’s focused attention to vaccinating new residents, this will be missed. And in the context of low staff vaccination rates, that would be a deadly mistake.
We MUST do better at reaching staff of nursing homes. Staff vaccination needs focused outreach, education, and engagement. Positive and negative incentives for staff can increase vaccine coverage. But at some point, there’s an ethical question.
A staff member who isn’t vaccinated may introduce infection that spreads throughout a facility and results in the deaths of many residents. This has been an issue with influenza vaccination for years; although there has been progress, still, only about two thirds of health care workers in nursing homes and other long-term care facilities get flu shots.
Thanks to @drgregpoland for raising the issue of health care staff vaccination for years. First must come making vaccination free, convenient, and sensitive, and addressing staff concerns. But at some point, staff choices may have lethal implications.
Vaccine News
There’s been a tsunami of information on vaccines in the past week. The Johnson & Johnson vaccine is promising: single dose, easy to handle, 85% protection against severe illness. Every new way to fight Covid helps. We can expect approval in February and increasingly widespread availability of this vaccine starting in April.
Interesting preliminary, pre-print data suggests that a single dose of the Pfizer and Moderna mRNA vaccines may be sufficient to provide protection in previously infected people. Practically, it would be difficult to get serology data in the contact of a mass vaccination program and so only give one dose to previously infected people, but this may be relevant for individuals. Again, it’s preliminary information and we don’t know how long the protection will last.
A single dose of the AstraZeneca vaccine has been reported to result in stable immunity for at least 3 months, but the data are messy and have not yet been peer-reviewed. The UK’s decision to delay the second dose of this vaccine is reasonable in the context of explosive spread of the predominant variant in that country, but we need much more data.
An approach from Russia using two different vectors also appears to be effective. Remember that old saying: Just because you’re paranoid doesn’t mean they’re not out to get you? Well, just because the data are dodgy, doesn’t mean that the vaccine doesn’t work.
Many different vaccine approaches are still being developed. China has a wide range of vaccines under development, ranging from inactivated, to vector (like the vaccines of AstraZeneca and Johnson & Johnson), to subunit (like the Novavax vaccine). Shouldn’t mRNA be considered a global public good for the benefit of all and widely available?
Thanks to Dr. Tony Fauci for the clear summary below of the different approaches being used for vaccine development in the United States. It’s amazing scientific progress – and also luck: Immunity is robust (unlike TB, malaria, HIV), and mRNA and adenovirus vector technologies were available just-in-time.
There’s also encouraging data from Israel. Vaccination of people over age 60 leads to big reductions (dark blue line in middle and right graphs) of severe illness. Vaccine programs must cover Palestinians in Israel and in the Occupied Territories, who face elevated risks. Disparities and inequalities must be fought everywhere they exist.
Variants threaten
So if we’re ramping up vaccination, and the proportion of people with immunity from infection (which, as another and very interesting study shows, is likely protective) is increasing steadily, what could possibly go wrong?
Variants, that’s what.
In Manaus, Brazil, the P1 variant has caused at least one reinfection. There’s not yet enough data to know if the rapid increase in cases in that city is due to reinfection among people previously infected with other strains (due to waning immunity or immune escape), increased transmissibility of this new variant, or some combination.
One line in a Novavax press release on the company’s South Africa trial reports reinfections with new variant, but provides no data. Tony Fauci provides another good summary of what we know about variants. One thing is clear: we need to pay less attention to individual variants and more to what the variants as a group are telling us.
The virus outnumbers us; we need to outsmart it. It’s in our self-interest to make sure the virus is controlled in the US and globally. With uncontrolled spread, more variants will emerge. And with increasing immunity from vaccine and natural infection, variants that evade these defenses, if they emerge, will spread. This could result in reinfections and also the spread of vaccine-escape mutant strains. Vaccines protect us. We must reduce spread to protect vaccines.
As Dr. Martin Luther King, Jr, said:
“Injustice anywhere is a threat to justice everywhere.”
Uncontrolled viral spread anywhere is a threat to viral control everywhere.
And ill health anywhere is a threat to health everywhere.
###
To Arms, To Arms! 1/30/21
There’s been promising news this past week. Cases in many parts of the country are decreasing, meaning there’s less spread. Hospitalizations are trending down. The Biden-Harris Administration has issued executive orders to speed action in our fight against Covid.
But there’s a long way before we can get control of the virus. In terms of vaccination, we must focus on 3 key things:
Get doses out of freezers and into arms ASAP. Vaccine does no good if it’s not given out. We need a strategy to make sure doses can be administered quickly as they become available.
Denominators: What percentage of nursing home residents and staff have been vaccinated? This is the highest risk group; vaccinating these people will sharply reduce spread in long-term care facilities and greatly reduce deaths, even if the overall number of cases in the entire population isn’t substantially reduced.
Improve equity. We need to do better at reaching Black, Latinx, Native American, and all underserved groups now. Racial and ethnic minorities experience disproportionately higher rates of hospitalizations and deaths. They also make up a disproportionately large segment of our front-line workforce – health care workers as well as store employees, delivery drivers, teachers, and everyone else who risks their health by keeping our economy and society functional.
How fast can vaccination help?
Some encouraging data from Israel. The more quickly we vaccinate, the more quickly we reduce deaths. How fast can vaccination against COVID-19 make a difference? Two weeks after 40% of those over 60 who had been vaccinated, the number of critically ill in the age 60+ group grew by 7% compared with the previous week’s growth of over 30%. There was less of a decrease in the growth of critically ill among the 40-55 age group – who were not as widely vaccinated as those over 60. If this trend continues, hospitalizations and deaths may already be dropping.
Better, but still bad
First, let’s get clear about the epidemiology and continued trajectory of the pandemic. Better does NOT mean good!!! In this case, it just means less terrible. The peak of hospitalizations in the prior two Covid surges in the US this past spring and summer was 60,000. Now we’re at 100,000. So our lower number is nearly double what it was at any prior peak.
Thanks to @NYTimes for working with @ResolveTSL to provide better and more actionable information on Covid risk in every community. Wide swaths of the country remain at extremely high risk, with only isolated pockets of low or even medium risk. http://nyti.ms/2MglGKu
I’m horrified to see so many communities opening up right now because they see that things are getting a little “better” when risk is still very, very high – as is the risk of new, more infectious, and potentially more deadly viral variants.
That sickening feeling. Imagine a punch-drunk boxer who has been knocked down twice, staggering up again to face an opponent winding up to deliver a knockout blow. That’s us, now, planning to open again because things are “better.” If communities open now, it’s not going to end well for far too many people.
Vaccine news
There have been a lot of scientific developments on vaccine, not all of of which are encouraging.
The Johnson & Johnson vaccine looks promising and likely to be submitted for approval to the FDA and approved soon. The J&J vaccine, a non-replicating viral vector vaccine that uses a common cold adenovirus and is designed to be given as a single dose, is about as good as a single dose of an mRNA-based vaccine.
In an @NEJM article from earlier studies, the immune response continued to build for 57 days after vaccination. Today’s results from the latest trial only show the effects 28 days after vaccination. The jury is still out on whether a second dose would be even more effective. https://bit.ly/3pJSquh
The J&J vaccine can be kept at regular refrigerator temperatures (no need for deep freeze) and is easier to make, store, ship, and give – at half the price. The company plans to manufacture a billion doses this year.
The Novavax vaccine, also soon to be rolled out, uses an engineered protein and an adjuvant, and is nearly as good as the mRNA vaccines. It’s nearly 90% effective at preventing Covid and, importantly, is effective at preventing severe cases. However, as is the case with other vaccines, it appears to be less effective (but not ineffective) against some of the newer and more transmissible strains, in particular the B.1.351 variant first identified in South Africa.
There’s a tantalizing line in the company’s press release that suggests that placebo recipients in South Africa who were seropositive at trial enrollment became infected with the new strain during the trial. SHOW US THE DATA! This is important and the world needs to know.
Data on study design, data, and effectiveness of the Astra-Zeneca vaccine are still murkier than they should be, and there are now production problems.
It’s possible that we’ll wind up with vaccines that may be relatively more and less effective. But the key is how well do they prevent people from developing illness severe enough to require hospitalization – and so far all of the vaccines seem to do that.
Adapt or else!
SARS-Cov-2 is evolving to adapt to the human context. As we develop vaccines and as more people become infected, the virus will mutate to evade our defenses. We may eventually need multivalent vaccines to fight these multiple strains. This wouldn’t be new. Vaccine protects against 3 different strains of polio, up to 9 of HPV, and up to 23 different pneumococcal strains. This could be where we’re headed with Covid vaccines, but it’s far too soon to know this for sure.
But the vaccines we have now work against strains that are circulating today. Things have gotten off to a bumpy start – this is the most complicated vaccination program in US history – but we have to get vaccines out of freezers and into people’s arms.
And we have to make sure that those who have been neglected so far – Blacks, Latinx, Native Americans, the poor, and, surprisingly, primary care doctors – are also prioritized to receive vaccines. First-come, first-served is a recipe to further exacerbate persistent inequalities.
Revealing description of the smoother roll-out in the UK, where they relied on their National Health Service and primary care doctors. Hope we’ll get the hint and strengthen primary care and make it central to our response.
Ramp up vaccination
We can use four platforms to get as many people vaccinated as quickly as vaccines are ready:
All health care systems
Mass vaccination clinics (there’s a great article describing how LA’s Dodger Stadium has been transformed into a high throughput vaccination center) – but it’s important not to reduce post-vaccination observation time to less than 15 minutes in case of very rare but potentially serious allergic reactions
Pharmacies (chains as well as independent pharmacies)
Pop-up, community-outreach sites set up anywhere they are needed that could be run by any of the first three.
The Biden-Harris Administration’s goal of vaccinating 100 million people in the next 100 days is ambitious and achievable – but the minimum of what we need to do. Vaccine supplies are short now, but will improve in the coming months. We will then need to parse everything we know about “underlying conditions,” using scientific and medical judgment and not just data, to prioritize those who will get the greatest benefit from vaccination.
There are about 81 million people in the US with high-risk health conditions. Some of these higher risk conditions are rare, so there won’t be much specific data about how Covid affects people that have them. CDC might consider subdividing these categories into those who are at very high risk and “only” at high risk, based not just on Covid-specific data but on review of all available scientific information.
Going back to nursing homes, if we’re successful, deaths that occur in these facilities will decline as a proportion of all deaths, then plummet dramatically during March. That would be a tremendous step forward. It’s impressive that 1.4 million long-term care residents have already received at least one dose of vaccine.
But we have to know the denominator – how many nursing home residents are there? And we have to do much better at vaccinating staff. There’s a lot of turnover at nursing homes, so we need to vaccinate every resident when they are admitted, as well as every new staff member as part of their onboarding.
There has been some resistance among workers at long-term care facilities, so we may need both positive and negative incentives to encourage staff vaccination. See the graph below and watch this space over the coming months.
Kudos to New York State for robust monitoring and reporting of vaccination data at nursing homes. Minnesota also has a good website reporting statewide data. Up next: Resolve and partners will be releasing recommended vaccine indicators this week as part of our initiative to provide accurate, recent, actionable data for responsible decision-making.
Protect our health care workers
We also need to make sure we #ProtectHealthWorkers as @AmandaMcClella2 and I wrote for @CNN. Countries all over the world have failed our caregivers for far too long. We must improve infection prevention and control in all health facilities, strengthen training and continued education so health workers can stay up to date on best practices, and provide socioeconomic, legal, and other support, as well as PPE of course, so they can continue to save lives when we need them most.
Also, in 2021, clean water, sanitation and hygiene (WASH) are not consistently available in about a third of health facilities worldwide. We must provide safe water for hundreds of thousands of health care facilities, among many areas of infection control where we need progress.
Vaccine nationalism
Vaccine nationalism – and failure to support developing economies with massive vaccination campaigns – is self-defeating. New financial modeling by @iccwbo warns of the cost of vaccine nationalism: $9.2 trillion, with nearly half, $4.5 trillion, incurred by wealthy economies including the United States.
A $27.2 billion investment on the part of advanced economies – the current funding shortfall to fully capitalize the global collaboration to accelerate development, production, and equitable access to COVID-19 tests, treatments, and vaccines – is capable of generating savings of $4.5 trillion, a return on investment as high as 166x.
Inequity causes crushing burdens on those people who are unfairly treated, but it also harms everyone. Uncontrolled disease spread anywhere is a risk everywhere. The only way through this is to scale up production, and this will require not only treating intellectual property as a global good but also vaccine production capacity.
One possible way forward would be to scale up mRNA manufacturing capacity in countries that have large populations and strong pharmaceutical sectors, such as Brazil, South Africa, India, and Vietnam. Because mRNA technology may be able to be used for multiple vaccines and other products in the future, this could be a regional and global benefit.
It will take time – which is why we should explore and consider starting right now. We need global collaborations that recognize the reality of our mutual dependency and mutual accountability.
5 points to wrap up
Lower doesn’t mean low. If floodwaters were over the roof of your house and now are up to the top-floor window, it’s still a flood. Especially if a hurricane (read: more infectious variants) may hit you soon. Until the worst is past, which won’t be for several morte months, we need to double down on protection protocols, including wearing masks and minimizing time indoors with people from outside your household.
Don’t focus on individual variants. What variants are telling us is the virus is wily: it can evade our defenses. We need better tracking of not just genomes but how they relate to epidemiology. More infectious variants will spread – that’s how natural selection works.
Masking is important. A mask not worn doesn’t protect anyone; any mask is a lot better than none. Better masks might reduce spread, but this is far from certain. Double masking, surgical masks, and N95/K95/KN94 masks all have theoretical benefits, but the key is to increase the proportion of time people wear ANY mask when they’re in an at-risk situation.
Improve implementation of our “Box It In” strategy to test/isolate/trace/quarantine, even if we can’t do much at the current sky-high levels of spread. When cases come down, we need to be ready to reduce spread even further through rapid isolation and effective tracing. This will help reduce emergence of escape-mutant strains and protect our vaccines so they continue to work.
Congress must act, and act quickly. Funds are needed to reimburse people for isolating or quarantining in order to prevent spread to others. For paid sick leave. For the US Public Health Job Corps. For schools to stay open more safely. For restaurants and bars to stay afloat while they are closed. To protect our country by improving global health security. And much more.
Today marks exactly one year since the first of these Friday evening Covid epidemiology roundups. It’s going to take a lot of hard work over the coming months to get control of the virus. But this time next year, I hope to be writing about our successes in stopping Covid and our progress improving our health care and public health systems so that we’ll be able to rapidly and effectively confront the next, inevitable threat.
Government in general, and public health in particular, at its best, is about the organized efforts of society to do what individuals cannot do or cannot do as effectively. It’s worth thinking back to the words and work of FDR’s great Labor Secretary, who was also the first female cabinet member and the longest-serving Labor Secretary:
“The people are what matter to government, and a government should aim to give all the people under its jurisdiction the best possible life.
Most problems have been met and solved either partially or as a whole by experiment based on common sense and carried out with courage.”
– Francis Perkins
Racing Against Mutants. 1/25/21
The post-holiday flood is cresting, but cases, hospitalizations, and deaths remain astronomically high. Viral mutants are increasingly concerning. Vaccination is our best tool, but only one of several we must use more and better.
Although the wave is cresting, last week cases (3x), hospitalizations (2x), and deaths were still far higher than at any point before the current surge. National test positivity decreased from 15% to 12%. A flood with receding waters is still a flood.
Reported cases don’t necessarily reflect community risk. For example, New York has a higher rate of Covid than Tennessee, but Tennessee tests at a rate that’s three times lower, with a much higher percent positivity. Tennessee is likely diagnosing a smaller proportion of its COvid cases than New York, which means the actual risk in the community is higher in Tennessee, even though reported case rates are lower..
Deaths are the key indicator—below is the trend around the U.S. since October. These numbers are SO high. If we mask and distance better we can drive cases down and hospitalizations and deaths will follow. The road ahead is long and bumpy and there are no shortcuts, but there’s a good new start.
New strains are more and more concerning. We are learning more about how Covid is evolving, and seeing changed in weeks and months. Did earlier clades spread then die out? New data from the UK suggest that the B.1.1.7 variant may be not only more infectious but also more lethal. Sometimes pathogens that jump the species barrier into humans adapt relatively quickly to their new host environment – us.
Credit to the UK for doing quick analyses showing that dexamethasone works, identifying the variant, and publishing important findings (such as on protection of health care workers by prior infection with SARS-nCoV-2) in real time. Doing real-time research in an emergency is hard but important. Now we need better studies, quickly, on the optimal dose and dosing schedule of the Oxford/Astra-Zeneca vaccine.
Vaccine rollout
Vaccination rollout stumbles along. I anticipate that we’ll get, for the first time, transparent information about the pace of future dose delivery. So far, 20 million doses have been given to 16 million people nationwide, including 2 million in nursing homes. Top performing states include West Virginia (8% coverage) and Alabama (4%).
Nursing home data is now on the CDC website, but there’s no denominator data. What proportion of residents and staff have been vaccinated nationally, in each state, and in each facility. The public has both a right and a need to know.
Some states are providing more comprehensive data on vaccine coverage, including Ohio, North Dakota, and Massachusetts, including data on race/ethnicity. We’re seeing rapid changes in data presentation and availability, and a national standard, pattern, and support would help.
The US will have too little vaccine supply for months. If people with prior documented infection who are not at high risk of infection/death choose to defer vaccination for a few months, this wouldn’t be wrong – but it must be their choice, and wouldn’t ease supply much.
New syringes to get the sixth dose out of Pfizer vials should be available soon. If there’s a real chance that a half dose of Moderna vaccine works, this should be studied rigorously even if studying this takes months. The new administration has demonstrated a good focus of partnering to get doses out of freezers and into arms.
Viral mutants
Here’s a crucially important risk: As immunity from infection and vaccination increases, selective pressure on the virus will favor emergence of strains that can reinfect people, and also strains that can escape vaccine-induced immunity. Never under-estimate the enemy.
We shouldn’t assume that more infectious strains will be less lethal. Strains that increase the duration of shedding would have an evolutionary advantage and might be more deadly. Instead of declining rapidly over the first week of illness, viral load might persist, increasing spread and also increasing risk to health care workers. This is just a theoretical possibility, but one example of the kind of change which evolutionary pressure might bring about.
The more uncontrolled spread of Covid there is, the higher the risk that mutants that can evade our natural defenses (immunity from either infection or vaccination) will arise and spread. So as we vaccinate, it’s EVEN MORE important we improve testing, isolation, tracing, and quarantine.
But we have to start with the brutal truth that the benefit of testing, isolation, and tracing in the US for the past year has been minimal. If we only find a third of people who are infected, isolate only a third of those before they spread the virus, and quarantine a third of contacts, we reduce spread by less than 5%.
Hope
Despite the bumpy road ahead, there’s hope. Vaccine supply and distribution will improve. Faster testing, rapid isolation with cash support and services, and expert forward and backward contact tracing with supportive quarantine can substantially reduce spread. This will help–along with masks, distancing, vaccination–drive the reproduction rate (Rt) to <1. It’s hard work, but possible and necessary.
Unfortunately, the pandemic is bad in much of the world and worsening in many countries. In parts of Africa there’s an impression that risks were exaggerated before; the future is uncertain. Disruption of health care systems remains a deadly consequence, especially in Africa where rates of death from conditions that are preventable or treatable is high.
Global solidarity is needed for global safety. I hope the virus will strengthen our understanding that our fates are intertwined.
The new administration has gotten off to a great start. Plan definitely beats no plan, and the Biden-Harris plan is clear and focused. Science is back, and there’s appropriate attention to organization, equity, communication, data transparency, and using all levers of government to fight the pandemic. So encouraging!
Truth is powerful and it prevails.
-Sojourner Truth
January 19: Could Covid Kill 1 Million Americans?
The rapid emergence of new coronavirus strains are a shot across the bow. It’s a message from the virus: We outnumber you. We’re more persistent than you. We change and adapt.
How we react to this shot across the bow is up to us. We must fight smarter, collaborate, and protect ourselves and each other better.
Epidemiology
First, let’s take a look at the numbers. Cases, hospitalizations, and deaths continue to increase, and, sadly, we can expect further increases. The scale of cases is mind-boggling. More than 1.6 MILLION cases were diagnosed last week, and that may represent, considering underdiagnosis, as many as a million new infections a day.
We may be seeing the beginning of a plateau of hospitalizations, but it’s too soon to be sure. If we could scale up infusion of monoclonal antibodies for people who are at risk for hospitalization but not yet very ill, we could reduce this number and decrease the stress on our health workers and health systems.
Health care workers continue to be avoidably and unacceptably at risk in the US and around the world. Resolve to Save Lives and partners released a report last week calling for global action to protect them. Banging pots is great, but providing the policies, support, and supplies health care workers need is a lot better.
Next week, I’ll delve into differences in Covid incidence among the states and explain why most comparisons you read are wrong. To start, look at the differences in testing rates by state. Incidence numbers are of little use without knowing testing intensity (which ranges from <100 to 10,000 per 100K) and the percent of PCR tests that are positive.
Epidemics are guided missiles attacking disenfranchised people. We need to do much better at addressing the deep inequities in society. Disproportionate impact of Covid means the need for disproportionate resources and support. Focusing on the hardest-hit communities isn’t just about fairness, it’s also about effectiveness.
A horrifying new projection shows that COVID-19 will reduce US life expectancy by 1.1 years, with reductions for Black and Latinx populations 3 to 4 times that, reversing more than 10 years of progress closing the Black-White gap in life expectancy.
New Viral Strains
Scientists continue to research and learn more every day about new strains of Covid. Data from the UK are clear: B.1.1.7 is more infectious, maybe 30%+ more. Strains from South Africa and the U.S. are likely also more dangerous. These strains demonstrate the evolution of a microbe that changes quickly.
More infectious strains require better defenses. That means not more of the same, but better of the same. I shared in Fox News the five things we must do to prevent a surge in Covid deaths.
Minimize time indoors with others not in your household.
Consider better masks. Surgical or N95, as available.
Accelerate vaccination.
Treat infections early.
Test, isolate, quarantine.
Bottom line: It’s not impossible that Covid could kill 1 million Americans. But it’s not inevitable either. This can happen, but only if we let it happen.
As I mentioned above, new variants are a shot across the bow. This scary study describes how the virus can become much more dangerous. “SARS-CoV-2 has the potential to escape an effective immune response and that vaccines and antibodies able to control emerging variants should be developed.”
Important point: More uncontrolled spread anywhere means more dangerous strains and higher thresholds for herd immunity. As we increase our immunity through infection and vaccination, the selective pressure on the virus will increase. This could result in a virus that can reinfect people more readily, or could escape vaccine-induced immunity.
Vaccination
In terms of vaccination, we’re making progress, but the rollout has been chaotic and the patchwork of policies has created avoidable confusion—a continuation of the marginalization of public health and the federal government’s lack of organization. The outgoing administration’s plan seems to be pointing fingers at states.
The only route to success is a whole-of-government, whole-of-society approach. If we’re divided, the virus will continue to conquer us. Vaccination won’t be quick or easy – this is the most complicated vaccination program in the history of the United States.
Fortunately, CDC’s website on vaccines has gotten better, and it’s encouraging to see that some states are doing well and making steady progress in long-term care facilities.
Vaccination prioritization should be straightforward:
All nursing home residents and staff
All healthcare workers with potential exposures
All people over age 65
All frontline essential workers.
That’s ~100 million people, ~200 million doses, but uptake will be less than 100%.
We will have too little vaccine until we have too much. We still don’t have enough transparency about how much vaccine is in the pipeline, from which companies, and when delivery is expected. There’s too little accountability or ability to plan. By March/April, we can hope to have additional authorized vaccines and supply.
Vaccination in nursing homes is crucial. By ensuring residents and staff get vaccinated, we can reduce death rates before we reduce case rates. By mid-February, the proportion of deaths from long-term care facilities should start to fall as a result of vaccination and in March, death rates should decline nationally. Currently, we have way too little data on how vaccination is progressing in these facilities.
Kudos to West Virginia (and credit to Dr. Clay Marsh and colleagues) for vaccinating more than 6% of the state population so far. The state has started vaccinations at all long-term care facilities. It also created a good vaccine dashboard (though it would be better if it compared vaccinations with the percentage of state population). If the US had given the same proportion of distributed doses as West Virginia, another 8 MILLION vaccines would have been given by the end of the week last week!
Primary care is also important for vaccination. Now, many primary care clinicians can’t even get vaccinated themselves! Data from Massachusetts shows the gap. The deeper issue is that we must fix the U.S. primary care system, in addition to fixing the U.S. public health system. More to come on this.
We should expect to see better information on who’s getting vaccinated. There needs to be more transparency on this and on the reasons for delaying the release of information. It’s understandable there’s missing data, but zip code data can help since, sadly, geography is usually a close proxy for socioeconomic status.
Some keys to successful vaccination programs:
Empower trusted community members and develop tailored messages
Provide reminders and ensure convenience (hours, locations, time)
Avoid hidden costs (for example, reimburse travel to vaccination sites)
Make vaccination the social norm
Anticipate and counter misinformation
Focus on personal, family, and collective benefits of vaccination.
Deaths
Remember the wisdom of William Farr: The death rate is a fact, all else is an inference. This graph shows very concerning death rate increases in the UK, Ireland (note shape of curve!), and South Africa. A more infectious virus means more infections, which means more deaths.
Thanks to the Wall Street Journal for analyzing excess deaths. This is important. Many excess deaths—most in some countries—are from Covid directly (likely Russia, Turkey, Mexico), and others are from disruptions (e.g. treatment of heart disease) caused by Covid (such as South Korea).
A Better Future
There’s good news. Vaccines are coming. We understand the virus and how to protect ourselves better. The US response is getting more organized, competent, and transparent. There’s more recognition that we’re all connected. The virus can catalyze community and global collaboration.
Don’t let your mask down. Don't let your guard down. Let’s learn, connect, and empower.
2021 can usher in a more connected, empathetic world.
“Only that day dawns to which we are awake. There is more day to dawn. The sun is but a morning star.”
– Henry David Thoreau
January 11: Humanity vs the Virus – the Virus is Winning
We’re facing a perfect storm: Uncontrolled spread in most of the US, slow vaccine rollout, and worrisome mutations that increase transmissibility and could undermine diagnostic testing, antibody treatment, and vaccine efficacy.
A misleading narrative suggests that uncontrolled spread of Covid shows that public health measures don’t work. The plain truth is that most places didn’t stick with the program long enough to get cases to a manageable level, and now masking and distancing aren’t being done reliably.
So yes, if you don’t use masks correctly and consistently, they don’t work. And vaccines don't work if people don’t take them. Fortunately, in terms of tracking where the virus and our response are, CDC data is getting ever more available and useful and the Covid Tracking Project remains invaluable.
Uncontrolled spread
The US is seeing record high cases, hospitalizations, and deaths – with continued increases. There’s a one- to two-week lag between cases and hospitalizations, as well as between hospitalizations and deaths. Expect continued increases in deaths in the days and weeks ahead. Scaling up antibody treatment might help, but, like vaccines, rollout has been botched. One bright spot is that there are an increasing number of effective treatments for Covid, including monoclonal antibodies early in the course of illness, and steroids such as dexamethasone late in the course of illness.
How stressed are hospitals? A new tool using HHS data shows the percentage of beds with Covid patients, which is a more reliable indicator than the percentage of ICU beds filled, since ICU beds can be added more easily than hospital beds (by converting surgical recovery suites, anesthesia rooms, etc). Anything over 15-20% of all beds filled with Covid patients is bad -- and that’s the situation now in much of the U.S.
But the limitation of beds isn’t the most dangerous, the limitation of staff is. Health care workers are exhausted and at risk. Relief is months away, and no reinforcements are likely to arrive from other parts of the country. That’s why it’s so important that vaccines get rolled out to health care workers quickly, and antibody treatments used to prevent hospitalizations in patients at risk for serious illness. Dr. Craig Spencer provides a vivid portrayal of these challenges here.
Why do some parts of the country have much more Covid than others? Rates of hospitalization range four to ten-fold among states. Fundamentally, there are four factors:
Opening too soon, leading to rapid resurgence
Failure to distance and mask
Failure to find and stop outbreaks
Superspreading events (bad luck).
In most places, public health measures didn’t fail – they weren’t applied. To a striking degree, this breaks down along partisan lines.
Look at Staten Island. The northern part, which is poorer and more Black and Latinx, has worse health outcomes and shorter life expectancy. But southern Staten Island, which is richer, whiter, and regularly votes Republican, has higher rates of Covid, including higher test positivity (~15% vs. ~10%).
We see similar differences, generally, between southern and northern California and the US South and North.
Humans take vacations but the virus doesn’t. Data scientist Youyang Gu shows in this thread that we’re nowhere near herd immunity.
As famed molecular biologist Josh Lederberg used to say, microbes outnumber us: it’s our brains against their numbers. Places like Vermont and Oregon are doing much better than others.
A reporter asked me the other day why California is doing as badly as Texas despite having more restrictions. That’s a faulty premise. If Texas had California’s death rate, 8,120 dead Texans would be alive today. And many places in California haven’t masked or distanced. There’s been a societal failure to implement public health measures.
Nationally, PCR test positivity rates are increasing steadily in 12-17 year olds and in 5-11 year olds, and are these groups have the highest test positivity of any age groups. Although imperfect, positivity rates are important to track – and this is not a good trend. Kids are seeding the virus throughout communities and the country.
Slow vaccine rollout
A second concerning trend is the delayed and uneven rollout of vaccines. Some of the challenges are understandable – the vaccines are new and difficult to store. Other challenges stem from incompetence. For example, the federal government has failed to support state and local microplans. Even for a competent government this would have been hard, and….
If vaccination is run like a grocery delivery rather than a comprehensive campaign, it won’t succeed.
Grocery delivery: temperature, restocking cadence.
Vaccination program: community engagement, microplanning, two-way communication, identification of trusted messengers and messaging in every community.
These are important but not well known documents about vaccination. Good CDC guidance, buried.
We also put together materials on how to plan for and communicate about Covid vaccination.
Here’s some plain talk on vaccines. They’re stunningly effective and, so far, reassuringly safe. The CDC shared some data behind the allergic reactions to Pfizer vaccine: there were 11 cases per million, 70%+ among people with a history of anaphylaxis or allergy. Among people without such a history, the rate is about 1/500,000.
Operation Warp Speed must stop hoarding vaccines!!! There’s no need to hold back half of the doses. Get them out fast. Although it’s possible manufacturers will miss their production targets, that’s a lesser risk than not flooding the zone ASAP with vaccines. (This is a different issue than the single dose issue in England, about which, more later.)
We should move to Phase 1C1 immediately (like, today) – vaccines should be made available to all 65+, all health workers, all nursing home residents and staff, and frontline essential workers. NEJM published some good information on how to promote vaccination. Bottom line: focus on making it convenient and on communicating with the movable middle.
Hint: the same folks who aren’t likely to wear masks are also not likely to get vaccines. We need to segment the market and target messages to different groups. The focus should be on getting back to normal, protecting jobs, and protecting our families. Demonstrate that despite a rocky start we’re making real progress.
There are still lots of unknowns regarding the AstraZeneca/Oxford vaccine. It may be less likely to give “sterilizing immunity.” Studies are urgently needed on the prime/boost approach to see if higher protective efficacy is confirmed. It’s reassuring that the data indicates fewer serious infections and no serious adverse events.
But...if it turns out that we have vaccines that are 70% effective (e.g., AstraZeneca, unless the prime/boost data is confirmed) vs. 90%+ effective, it’s going to raise terrible questions. Scientific knowledge should be in the public domain. It's a moral imperative to make the best vaccines for the most people.
New strains
Now, if uncontrolled spread and slow vaccine rollout didn’t alarm you, let’s talk about new strains of the virus. At first I thought maybe the UK was blaming mutations for sloppy public health work – but no. The strain really is more transmissible. It’s not inevitable that it will spread in the US, but it’s likely.
I've never seen an epidemic curve like this one. If the variant becomes common in the US, it will be close to the worst-case scenario, with a baseline of full hospitals. (Not worst case: case fatality rate is about 1/200, worst case could be 1/10 or even higher.) The strain has the potential to create a perfect storm, especially with political turmoil and a leadership vacuum.
What’s happening in Ireland is deeply concerning. In just a few weeks, the new strain has gone from making up less than 1 in 10 new cases, to nearly 1 in 4 new cases. We could use more data to understand this better, and the relaxation of indoor restrictions undoubtedly helped, but the trend is ominous.
Let’s be clear: new strains will continue to emerge, as they do with most viruses. B.1.1.7 is more transmissible, so it will cause more infections, hospitalizations, and deaths. Strains may emerge that make testing less accurate, treatment less helpful, or vaccines less effective. B.1.1.7 is a shot across the bow. Covid will be with us for years.
So far, we’ve failed at controlling Covid in the US. Now if a more infectious strain takes hold, we’ll have to do so much better. We’ll have to curb avoidable indoor exposures. Maybe, wear better masks. Although we should definitely not change the vaccine dose schedule now, if we get to a UK-like situation, it has to be considered.
We have another nine days of absent leadership and active undermining of lifesaving public health measures. These days are so very dangerous, for so many reasons, including the potential for exponential growth of the B.1.1.7 strain.
Many years ago, Senator Moynihan said, "Everyone is entitled to their own opinion, but not their own facts." That should not be too much to ask. We need to get back to that perspective, urgently, to protect ourselves and our families.
This long article on the impact of Covid on young Black men is a must-read. As I think about 2020, I mourn the 400K+ deaths in the US (that’s the accurate number considering excess mortality), many of which were preventable. But I will also never forget – and do not want to forget – the horrific, lynching-like killing of George Floyd.
“Concern for man and his fate must always form the chief interest of all technical endeavors. Never forget this in the midst of your diagrams and equations.”
– Albert Einstein
December 21, 2020
Covid Epi Weekly: First Sighting of Vaccine-Induced Immunity
Imagine you’ve been on a dangerous sea voyage. One of 200 people over the age of 65 have perished as have many others. Safe land is sighted in the distance. Everyone on board must do everything possible to reduce deaths until safe harbor is reached.
At this stage of the pandemic, we’re facing a tale of two realities. On one hand, the U.S. is experiencing the worst spread of Covid since pandemic started. Cases, hospitalizations, and deaths continue to set records. At the same time, the rollout of highly effective, safe vaccines has given us the most hope we’ve had for a beginning of the end.
First, let’s discuss the latest epidemiology. It’s great that CDC and HHS have FINALLY been allowed to release some of the information they have. This information belongs to the public, not to anyone in Washington. It’s 10 months late, but the headline says it all.
Unfortunately, what the data shows is NOT great. Every U.S. region and most counties for which there are data are at the highest level in terms of case incidence — more than 200 cases per 100,000 a week. That’s about six times the rate at which we figured contact tracing would be hard or impossible.
Counties across the US are sustained hotspots, meaning there is a high case burden and a risk of overwhelming health care systems. Here’s the point: the longer you delay closures, the longer you have to keep things shut, the higher the risk of overwhelmed ICUs, and the more people die.
Hospital beds are being filled by Covid patients. There were 156,000 admissions in the past week and there are more than 113,000 people currently hospitalized. Cases are still increasing, and a further increase in hospitalizations will follow. Note the increase after Thanksgiving in most regions.
This post-Thanksgiving bump is evident in cases and test positivity. With December holidays coming, it’s best to celebrate at home. When people travel, the virus travels. When people share air, the virus spreads. Not every state had a bump — protection protocols save lives.
Now that this CDC and HHS information is finally public, it’s clear what’s happening. There are very high rates in most of the country, but much of the country has seen decreases over the past week, particularly the Upper Midwest. The Thanksgiving surge is ebbing, just in time for the next holiday surge. Tennessee has become a new hottest spot: deeply red, deeply concerning.
It’s worth focusing on the graphic below, which gives a sense of both test positivity and trend. States all over the map are … all over the map. Some states are high and increasing, some are high and decreasing, some are staying high, and some are staying low. Hawaii, Vermont, and Maine are the Covid-safest places in the United States to be today.
Farewell and thanks to Covid Exit Strategy, which provided excellent data and visualizations of the state of the pandemic in the US. Welcome Covid Act Now, which will be taking its place. However, if CDC and HHS continue to improve their data sharing, these sites — and this weekly thread! — will become unnecessary. (I’d like that a lot!) Communication, based on facts, is an essential weapon to fight the pandemic.
Now for the view of the safe harbor — vaccine-induced immunity. It’s coming, but there will be barriers: production, distribution, adverse events, uptake, and more. It won’t be fast or easy, but it will happen. Two authorized vaccines are good, four authorized vaccines will be better. More are coming next year.
Production is a big unknown. Johnson & Johnson is the only company that has extensive vaccine production experience of the first four companies likely to have a vaccine. We can expect adverse events -- some related to vaccines, some not. Complete transparency and immediate communication are both essential.
There’s not enough vaccine now, so we MUST do better protecting the most vulnerable. There have been horrific outbreaks and deaths in nursing homes, the grim harvest of misguided advice to let infections spread among young people. Monoclonal antibody treatment must be scaled up fast. It’s simply inexcusable that this isn’t happening.
It’s misguided to debate whether the elderly or essential workers should get vaccinated first. Essential workers who are more likely to be infected and die (for example, a bus driver with diabetes) should also be at the front of the line. But an 85-year-old is at massively higher risk than a 65-year-old. Granularity can help de-conflict. ACIP guidelines released over the weekend are sensible and thoughtful; key will be fair and effective allocation. The beginnings of would could be one encouraging example from Tennessee.
Outbreaks and deaths among incarcerated people continue. Sensible decarceration is a public health and ethical imperative. A prison sentence shouldn’t be a death sentence.
We’ve made some progress on global vaccine access -- potentially 2 billion doses will be made available to countries through COVAX. More doses, more money, and more support for vaccination programs are all needed. Ironically, many countries last on line for the vaccine have vaccination systems that are best able to deliver it.
It’s literally now or never to fix public health at local, city, state, national, global levels. If this isn’t a teachable moment, there will never be one. Vaccination may end this pandemic, but not the risk of pandemics. Money, technical capacity, and operational capacity are all needed.
We must work together to make 2021 the year the world got serious about preventing pandemics.
So we come to the end of my last weekly analysis of this awful year. We’re in this world together. Those who die diminish us all. Those who build community strengthen us all. Seasons and years pass.
What could possibly be more important than preventing disability and death?
“As are generations of leaves, so are those of humanity.
The wind scatters leaves on the ground, but the trees burgeon
With leaves again when the spring season returns.
So one generation of people will rise while another dies.”
Homer, The Iliad
December 14, 2020
Covid Epi Weekly: First Sighting of Vaccine-Induced Immunity
Imagine you’ve been on a dangerous sea voyage. One of 200 people over the age of 65 have perished as have many others. Safe land is sighted in the distance. Everyone on board must do everything possible to reduce deaths until safe harbor is reached.
At this stage of the pandemic, we’re facing a tale of two realities. On one hand, the U.S. is experiencing the worst spread of Covid since pandemic started. Cases, hospitalizations, and deaths continue to set records. At the same time, the rollout of highly effective, safe vaccines has given us the most hope we’ve had for a beginning of the end.
First, let’s discuss the latest epidemiology. It’s great that CDC and HHS have FINALLY been allowed to release some of the information they have. This information belongs to the public, not to anyone in Washington. It’s 10 months late, but the headline says it all.
Unfortunately, what the data shows isn’t great. Every US region and most counties for which there are data are at the highest level in terms of case incidence — more than 200 cases per 100,000 a week. That’s about six times the rate at which we figured contact tracing would be hard or impossible.
Counties across the US are sustained hotspots, meaning there is a high case burden and a risk of overwhelming health care systems. Here’s the point: the longer you delay closures, the longer you have to keep things shut, the higher the risk of overwhelmed ICUs, and the more people die.
Hospital beds are being filled by Covid patients. There were 156,000 admissions in the past week and there are more than 113,000 people currently hospitalized. Cases are still increasing, and a further increase in hospitalizations will follow. Note the increase after Thanksgiving in most regions.
This post-Thanksgiving bump is evident in cases and test positivity. With December holidays coming, it’s best to celebrate at home. When people travel, the virus travels. When people share air, the virus spreads. Not every state had a bump — protection protocols save lives.
Now that this CDC and HHS information is finally public, it’s clear what’s happening. There are very high rates in most of the country, but much of the country has seen decreases over the past week, particularly the Upper Midwest. The Thanksgiving surge is ebbing, just in time for the next holiday surge. Tennessee has become a new hottest spot: deeply red, deeply concerning.
It’s worth focusing on the graphic below, which gives a sense of both test positivity and trend. States all over the map are … all over the map. Some states are high and increasing, some are high and decreasing, some are staying high, and some are staying low. Hawaii, Vermont, and Maine are the Covid-safest places in the United States to be today.
Farewell and thanks to Covid Exit Strategy, which provided excellent data and visualizations of the state of the pandemic in the US. Welcome Covid Act Now, which will be taking its place. However, if CDC and HHS continue to improve their data sharing, these sites — and this weekly thread! — will become unnecessary. (I’d like that a lot!) Communication, based on facts, is an essential weapon to fight the pandemic.
Now for the view of the safe harbor — vaccine-induced immunity. It’s coming, but there will be barriers: production, distribution, adverse events, uptake, and more. It won’t be fast or easy, but it will happen. Two authorized vaccines are good, four authorized vaccines will be better. More are coming next year.
Production is a big unknown. Johnson & Johnson is the only company that has extensive vaccine production experience of the first four companies likely to have a vaccine. We can expect adverse events -- some related to vaccines, some not. Complete transparency and immediate communication are both essential.
There’s not enough vaccine now, so we MUST do better protecting the most vulnerable. There have been horrific outbreaks and deaths in nursing homes, the grim harvest of misguided advice to let infections spread among young people. Monoclonal antibody treatment must be scaled up fast. It’s simply inexcusable that this isn’t happening.
It’s misguided to debate whether the elderly or essential workers should get vaccinated first. Essential workers who are more likely to be infected and die (for example, a bus driver with diabetes) should also be at the front of the line. But an 85-year-old is at massively higher risk than a 65-year-old. Granularity can help de-conflict. ACIP guidelines released over the weekend are sensible and thoughtful; key will be fair and effective allocation. The beginnings of would could be one encouraging example from Tennessee.
Outbreaks and deaths among incarcerated people continue. Sensible decarceration is a public health and ethical imperative. A prison sentence shouldn’t be a death sentence.
We’ve made some progress on global vaccine access -- potentially 2 billion doses will be made available to countries through COVAX. More doses, more money, and more support for vaccination programs are all needed. Ironically, many countries last on line for the vaccine have vaccination systems that are best able to deliver it.
It’s literally now or never to fix public health at local, city, state, national, global levels. If this isn’t a teachable moment, there will never be one. Vaccination may end this pandemic, but not the risk of pandemics. Money, technical capacity, and operational capacity are all needed.
We must work together to make 2021 the year the world got serious about preventing pandemics.
So we come to the end of my last weekly analysis of this awful year. We’re in this world together. Those who die diminish us all. Those who build community strengthen us all. Seasons and years pass.
What could possibly be more important than preventing disability and death?
“As are generations of leaves, so are those of humanity.
The wind scatters leaves on the ground, but the trees burgeon
With leaves again when the spring season returns.
So one generation of people will rise while another dies.”
Homer, The Iliad
With the first doses delivered this morning, the first step on the road to immunity through vaccination has been taken. At the same time, we’ve seen a deeply discouraging lack of action to stop the pandemic. The coming weeks will be devastating, but I fear that numbness to suffering is spreading as rapidly as the virus.
First the good news. The FDA has provided good transparency about vaccines and the data is about as good as could be. The vaccines are highly effective, including for older people (though few frail elderly were included in the studies), and against severe infection. We haven’t seen any serious adverse events, but we need to track for this when millions are vaccinate
The road ahead for vaccination will be bumpy. Production, supply, distribution, uptake, and possible adverse events—all present potentially huge challenges. New vaccines from other companies will likely be approved in the New Year. The vaccination campaign will be an enormous challenge, but if the communication is done well, it can succeed.
Unfortunately, we’re not there yet. It will be months before most people can get vaccinated. We must double down on protection protocols. The post-Thanksgiving surge is driving rates up, and December holidays could bring new horrors at the start of 2021. I fear we are numbing to the numbers.
Cases continue to increase, hospitalizations are at highest rate ever, and deaths are continuing to hit new highs. It’s horrifying to see a 13% test positivity rate nationally, with 40 states reporting positivity rates greater than 8%. Although cases in the Midwest are coming down, they’re still very high, and cases are increasing almost everywhere else.
It gets worse. Covid has exposed horrific disparities. In Rhode Island, more than 1 in 8 Hispanic/Latinx people has tested positive, which is nearly 4x the rate among white people (1 in 31). In the Dakotas, 1 in 8 Black people has tested positive. In South Dakota, 1 in 7 Native Americans has tested positive.
Global disparities will worsen in 2021. Countries in Africa have fragile health systems that can be quickly overwhelmed by Covid. As vaccination rolls out in richer countries in 2021, will healthy people in the US get vaccinated before health care workers and nursing home residents in Africa? That would be indefensible. There are just a few million health care workers in Africa. They should be at the front of the global line — there’s already a terrible shortage of health care workers on the continent.
As 2020 draws to a close, the next few months will determine our future. These are some of my takeaways from a year of horrors:
We must remember that public health is fundamental to society
Science is as vulnerable to politics as humans are to viruses
We will look back and ask why we didn’t do more.
We can control our health, but only if we work together. (Look at the enormous difference cooperation makes — see the two graphs below.)
We just released materials to promote safer holiday celebrations. By being careful now, we’ll have more to celebrate and less to regret in the new year. Being in a bubble or pod is an important concept, but each bubble is only as strong as its weakest part.
As German Chancellor Angela Merkel said, patience, discipline, and solidarity are key. These three characteristics are essential for a successful response. We are inextricably connected. Empathy gives us the sense of others’ suffering, joys, and losses.
“The death of human empathy is one of the earliest and most telling signs of a culture about to fall into barbarism.” — Hannah Arendt
###
Navigation Home Images Scientific publications News Q4 2020 News Q3 2020 News Q2 2020 News Q1 2020 News Op-Eds Media Videos Tom Frieden - Media Interviews Tom Frieden - CDC Ebola Modeling Blog
Cases are increasing exponentially in most of the US. The current epicenter is the Midwest. Diagnosed cases have been in the 150,000–200,000 range, but there are likely at least half a million new infections each day. In South and North Dakota, an estimated 1 in 11 people have Covid. This figure from the Covid Tracking Project shows key trends.
As per CDC’s CovidView weekly, test positivity, which remains one of the most important indicators of disease spread, increased from 10.8% to 11.9%. One of the analysts I follow closely is @youyanggu, who just launched a nowcasting site. He estimates that there are 3.3 infections for each diagnosed infection. In other words, the case detection rate (CDR) — the proportion of all infections diagnosed — in approximately 30%. The CDR is difficult to estimate, but it is very important, and I’ll return to this topic in the future article.
Although not all people who are estimated to have illness are infectious (maximum infectivity starts about 2 days before and continues for about 5–7 days into illness), nationally approximately 1 in 100 people, and possibly more, are infectious today. The analysis and map by Youyang Gu https://covid19-projections.com gives estimates.
The US has the highest rate of hospitalizations from Covid ever. Deaths are increasing. Further increases inevitable — but continued increases are not (more on this later). Excellent graphic from the folks at Covid Tracking Project. Midwest is having a crescendo. Cases in the Northeast are increasing. In the South, cases never decreased much, and now are increasing. Cases in the West are increasing https://bit.ly/3kQONPy
Hospitalizations are increasing steadily. Already many are stretched; it’s likely we’ll see another 30,000+ increase in coming weeks, increasing from 70,000 to 100,000. The scarcest resource: trained healthcare staff. PPE remains insufficient. Nursing home cases are increasing. And all of this will get worse. 4/10
If our plans don’t change, Thanksgiving will be the Super Bowl of super spreader events, accelerating an epidemic already out of control. Good guidance from CDC. Better a Zoom Thanksgiving than an ICU Christmas. Read my latest op ed about where we are and what we can do for the holidays. At Resolve, we created the graphic below — important to understand that degrees of separation and connection are much broader than we realize.
In President Obama’s book, he writes:
“The pandemic we’re currently living through is both a manifestation of and a mere interruption in the relentless march toward an interconnected world.”
There’s continued and very encouraging news on vaccines. But there are still many unknowns. It remains to be seen how rapidly supply will increase, how long immunity will last, whether there will be strong protection of frail elderly people such as many who are in nursing homes, and whether there will be rare safety problems identified when millions of people are vaccinated. And as distribution begins, it will need to be fast, fair, and transparent. Nursing home staff and residents should get first, and it’s encouraging that the current administration seems to be planning for this. It’s crucial that there be a smooth handoff to the incoming Biden administration — this is going to be the most complicated vaccination program in the history of the United States. Good report by the Kaiser Family Foundation, with some key findings below. States have made some progress but much more is needed, and states need money to prepare and implement. Congress must act.
A vaccine won’t be widely available for many months — so we need to have much better control for many more months. The New York Times has a GREAT graphic presentation showing that policy matters.
Here’s a sad tale of 2 states. Vermont is 6 times more densely populated than South Dakota, but has 16 times fewer cases and 10 times fewer deaths. Following science saves lives. I outlined how we can make progress using a one-two punch strategy with more nuanced closures and more effective testing and isolation.
Hong Kong and Singapore created a travel bubble. If there are more than 5 unlinked infections per day, they will stop travel. Yesterday there were approximately 500,000 unlinked infections in the US — an astounding 100,000 times more. With a new approach based on science, organized response, and honest communication, together we can make steady progress.
Masks and mask mandates work! Important report from CDC. Impressive graphics — the line graph is worth careful study. Freedom includes freedom from disease. That should not be hard to understand.
I wish you all a happy, socially connected, physically distanced Thanksgiving!
“Wear gratitude like a cloak and it will feed every corner of your life.
― Rumi1 LIKES SHARE
(Article initially published on Tom Frieden’s LinkedIn: https://www.linkedin.com/pulse/covid-epi-weekly-death-wont-take-holiday-season-tom-frieden/)
We have a divided government and a divided country, just when we most need unity to stop the pandemic. Covid is skyrocketing across the country, but some areas are being hit much harder than others. Correcting for how much testing is done, there’s a 100-fold difference between South Dakota and Vermont and 10-fold difference between the Northeast and Upper Midwest.
How bad is the increase we’re seeing? Bad. Cases are doubling, tripling, or more in many communities and states. Much of the US is in the exponential increase phase, and every day of delay costs lives. The basic 1-2 punch concept still applies. 1) Knock the virus down, minimizing societal harm, and 2) Keep it down.
First, let’s take a look at the numbers. They’re bad almost everywhere. According to the CDC, national percent positivity increased (from 7.2 to 8.2%), and increased among all age groups in all regions. Horrifying. This is a national tsunami. Hospitalizations are up 14% and deaths up 8%. Deaths follow hospitalizations by a week or two. These numbers will continue to rise.
Many thanks to Covid Exit Strategy for their great work tracking the situation in each state. I hope the site, and others, like it, will be put out of business by a competent federal response that gets us all on the same page and demonstrates that our only enemy is a virus. The more we work together, the more we can control Covid.
The increases in hospitalizations required the Covid Exit Strategy team to add a new color. The Upper Midwest is in the exponential increase phase. Here’s the key point: the per capita hospitalization rates for Covid range from 500 per million to <50/million. That’s a 10-fold difference. Policy matters! Covid can be controlled.
It’s been frustrating to see a continued focus on the wrong numbers. Detected cases are only about one fifth of total infections. A weighted ranking of test-intensity and incidence helps. As I mentioned at the beginning of this post, there’s a 100-fold difference between South Dakota and Vermont.
We’re waking up to the fact that we need to shut down. We can do this sensibly, keeping schools, childcare, universities, shopping, barber shops, and other places open—but ONLY with rigorous safety measures and modifications. We will need to reduce travel and risky indoor gatherings. Ireland’s approach is a great example.
Like oh-so-much-too-much in our society, Covid hurts the most vulnerable most. Rates of infection are vastly higher in Native American, Latinx, and Black communities. The virus doesn’t stay in any group—we’re all connected. The more safe we all are, the more safe we all will be.
Sooner or later, we’ll have to knock down the spread of the virus with strategic closures. But we need to vastly up our game in preventing household spread.
A stunning study found a very high attack rate among children in families with Covid: 77%! 
Other studies have found lower rates, but the bottom line is not finding people who are infected fast and helping Covid patients relocate during maximum infectivity extends explosive spread by weeks or months. We must reduce the time from infectivity to isolation, offer paid sick leave for all, and make isolation more effective. Knocking down spread is the first punch, boxing the virus in when new infections emerge is the second punch.
We must discover more, such as how to avoid leaving infectious people at home, how to best use the tens of millions of antigen tests being sent out, and how to scale production of N95 (including safely reusable) and surgical masks.
Pandemic fatigue is understandable. We all feel it. The WHO Euro released a helpful report showing how we can help address it:
● Understand and empathize
● Engage communities to find solutions
● Reduce restrictions but protect lives
● Be transparent, consistent, predictable, and fair.
The virus isn’t giving up, and neither can we. Success is possible. It takes rigor, discipline, patience, and working together. This CDC article shows the positive impact of targeted closures and widespread use of masks.
The sooner we shut, the softer and shorter we can shut. We can minimize disruption to holiday shopping, jobs, education AND reduce major drivers of spread. To have happier holidays, we need to stay much safer for the next six weeks.1 LIKES SHARE
(Article initially published on Tom Frieden’s LinkedIn: https://www.linkedin.com/pulse/covid-epi-weekly-harrowing-holidays-tom-frieden/)
It’s hard to imagine a worse confluence. Cases are surging in much of the US. People are tired of the limitations the virus is imposing. Economic harm is real, painful, and persistent. And White House communications have continued to mislead, divide, and deny.
Bottom line (almost) up front: there IS one thing that can stop Covid. For months I’ve said there isn’t one thing, but there is. Not masks. Not travel limitations. Not staying home. Not testing. Not contact tracing. Not isolation. Not quarantine. Not even a vaccine.
It’s TRUST.
Around the world, the best predictor of controlling Covid is social cohesion: the understanding that we’re all in this together. We’re all safer when we all mask up, stay home when we’re sick, support contact tracing, and, eventually, get vaccinated. No group can get the infection without endangering other individuals and groups.
That’s why the unspoken advocacy for herd immunity by this White House is so revealing. “Protect the vulnerable” sounds great. But doing that while allowing the virus to spread among the young is an impossibility. It’s a scientific blunder emanating from a philosophical error.
When we understand we’re all connected, we can win. Let’s prioritize getting services to people and communities most in need. Let’s protect ourselves, our families, our community. There’s only one enemy: a virus. White House divisiveness is the best ally the novel coronavirus could possibly have.
Now, the disheartening numbers. Detected cases are up three times more than testing. Testing is up 8.6%, while cases are up 24%. What’s more, test positivity has risen from 6.6% to 7.1%. Saying cases are up because of more testing is like saying gravity isn’t real. This is an informative, though depressing graphic from The Covid Tracking Project.
Here’s a good way to show that cases are increasing much faster than testing by state. Case growth has been much higher than test increases in all states. (The published data from Mississippi has been whipsawing.)
Reported cases fluctuate by day. Generally, see lower case numbers over the weekend because of fewer office visits and tests. The weekends are time off for many people, but not for the virus. Paying attention to the seven-day average of reported cases is more useful.
Hospitalizations are, of course, increasing following case increases. It’s shameful and inexcusable that the federal government is not publishing data it has on the pandemic. NPR obtained a recent daily report from the US Department of Health and Human Services, and here’s a screenshot showing hospitalizations increasing:
Will deaths increase? Does night follow day? Of course. We ardently hope that deaths won’t increase as much as in the past, due to better care, fewer overwhelmed hospitals, and the use of dexamethasone and possibly other treatments. But only time will tell. Deaths follow case increases by about three weeks.
Wisconsin is a bellwether … including for Covid deaths. The state has seen a huge increase in Covid deaths. Many other states, sadly, aren’t far behind. 
As an epidemiologist, I think a lot about numbers. This week, two numbers made a big impact on me: 13 and 9.
● 13 is the number of years of life lost on average for each of the 230,000+ Americans killed by Covid.
● 9 is the number of people, on average, grieving for each of those deaths.
These represent millions of tragedies, most of the preventable.
We public health specialists must never underestimate the health and social impact of economic harm. We’re heading into a dark winter. We can limit harm with more outdoor activities, open schools, social connections, and shopping. And by reducing indoor maskless contact in poorly ventilated spaces.
I’ve shared some bad news so far. Here’s some good news. 9 of 10 people understand the importance of masking up. Those who don’t are a small, misguided minority. Masking up correlates well with lower case counts. Mask mandates, if done well, boost mask use and save lives.
The increase in telemedicine is also good news. Primary care is the most important part of our health care system, but it’s also the most underfunded and neglected. If we get regulation and reimbursement right, telemedicine will be an important part of fixing primary care and our health care system.
An interesting data survey summarized by Covid Exit Strategy shows that in states with more than 90% mask wearing, less than 20% of people know someone who is sick. In states with 80% or less mask wearing, 30-54% know someone who is sick. Look at the top and bottom places here—the gap is striking!
One of the many, many failures of this administration’s response to Covid has been insufficient protective equipment for health care workers. It makes me SO ANGRY. We’re sending our troops into battle without the armor a competent government would have provided.
Case increases lead to a vicious cycle: longer test turnaround, overwhelmed public health, less isolation of infected patients, more cases. If we reduce cases by wearing masks, watching our distance, washing our hands, and avoiding risky indoor spaces, we can create a virtuous cycle: fewer cases, better contact tracing, and enhanced ability to stop spread.
Why harrowing holidays? Thanksgiving in Canada. The country has struggled with case increases, division, attempts to undermine science, and denials of reality. Even countries which have done relatively well are now struggling. The US, with a completely failed federal response, faces potential devastation.
“Ending the COVID-19 pandemic”? The claim in this White House letter is Orwellian.
The reality is the pandemic won’t end anytime soon. But maybe, soon, there will be an end to the completely dysfunctional national response.1 LIKES SHARE
October 23, 2020. You know what’s NOT tired of winning? Covid. Covid’s not tired of winning. Unless we up our game, Covid will keep winning, keep spreading, keep killing Americans—preventably.
Test positivity is increasing in ALL age groups. Positivity in people over the age of 65 increased from 3.6% five weeks ago to 5.2%—a 44% increase. Five weeks ago, the rate in young adults was 50% higher than in those over 65; last week the rate was just 20% higher. This confirms that what started in the young didn’t stay in the young.
Cumulative hospitalizations for adults over 65 in the US:
1 in 300 White people
1 in 120 Native American people
1 in 110 Latinx people
1 in 87 (!) Black people.

The emergence of Covid has exacerbated racial injustice in health. Black and Latinx communities already had less access to health care. The inadequate protection of essential workers, many of whom are Black/Latinx, has also magnified inequities.
Years of life lost is a good way to measure the burden of a public health crisis, though it’s far from perfect. There have already been 2.5 million life years lost, more than 13 years for every one of the 225,000 people who have died from Covid. Think of the joy, happiness, and meaning lost for each of those 13 years. Each of those 2.5 million years.
A working paper published in June by former NYC Health Commissioner Dr. Mary T. Bassett showed the same pattern: Black and Latinx people in the US make up 33% of adults but 74% of early death. This is horrifying. Valid responses to this information include rage and action.
Other than Northeast, this map is bleak. 
Although it’s clear that there is a worsening situation in the US, we’re flying blind as to exactly how and where Covid is spreading. Test positivity is less informative than it was before. Case rates are an even worse indicator. The record 85,000 infections reported for Friday represent only about 20% of all infections. The failure of federal leadership means we’re not tracking the right indicators.
Take a look at the Dakotas. Neither state has a mask mandate. They are losing to Covid. The reported rates are slightly higher in North Dakota (1,000 vs. 800 per million a day), but when corrected for test intensity, South Dakota has about 4x the rate of North Dakota and 20x the rate of the Northeast. In other words, South Dakota looks not as bad, but it’s actually much worse.
Rural areas are getting slammed. These graphs from the New York Times show this clearly. Meat packing and agricultural outbreaks are part of, but only part of, the factors driving the increase. No place is immune to Covid.

Increasing cases in Alaska suggest that colder weather may favor the virus. In the classic Art of War, Sun Tzu defined five factors that determine success or failure in war: moral influence, weather, terrain, leadership, and strategy. In our war against Covid, the US is not organized for success in any of those 5 - we’re zero for 5 at present.
Parts of Europe are also getting hit hard. Places that didn’t drive cases down enough to find and stop clusters face the ever-present risk of explosive spread. Some countries didn’t flatten the curve sufficiently (Spain, France, Italy, UK, Belgium) and some did (Germany, Norway, Finland).


Economic pain is real, and deadly. We are all impatient to resume activities we miss, but the reality is there are things we won’t be able to do until we control the pandemic. Here’s more evidence the virus, rather than control efforts, is what’s suppressing economic recovery. “It has almost nothing to do with regulations.” Paraphrasing James Carville, to fix the economy, it’s the pandemic, stupid.
Balance is key in our response. We must apply more granularity to our “circuit breakers” to stop Covid. Yes, we’ll have to adapt our lives for the foreseeable future. But there are a lot of activities we can and should do, while taking steps to reduce risk. Schools, healthcare, workplaces, stores can open more safely. Spending time outdoors is great. On the other hand, travel from places with high Covid to places with low Covid is a recipe for spread. Restaurants, bars, and indoor get-togethers amplify the virus and we’ll need to figure out how to do this as safely as possible.
The higher the peak, the longer it lasts. The lower Covid goes, the longer it takes to come back. As we sow, so shall we reap. Hyperbolic discounting is not in our favor here. As night follows day, hospitalizations and deaths follow cases, which follow letting our guard down.
Civic responsibilities include not harming (e.g., infecting with coronavirus) others, staying informed, paying taxes, participating in your community. And VOTING. We released materials on voting more safely. I like the message below. Please spread the word.
Covid Epi Weekly: Harrowing Holidays
It’s hard to imagine a worse confluence. Cases are surging in much of the US. People are tired of the limitations the virus is imposing. Economic harm is real, painful, and persistent. And White House communications have continued to mislead, divide, and deny.
Bottom line (almost) up front: there IS one thing that can stop Covid. For months I’ve said there isn’t one thing, but there is. Not masks. Not travel limitations. Not staying home. Not testing. Not contact tracing. Not isolation. Not quarantine. Not even a vaccine.
It’s TRUST.
Around the world, the best predictor of controlling Covid is social cohesion: the understanding that we’re all in this together. We’re all safer when we all mask up, stay home when we’re sick, support contact tracing, and, eventually, get vaccinated. No group can get the infection without endangering other individuals and groups.
That’s why the unspoken advocacy for herd immunity by this White House is so revealing. “Protect the vulnerable” sounds great. But doing that while allowing the virus to spread among the young is an impossibility. It’s a scientific blunder emanating from a philosophical error.
When we understand we’re all connected, we can win. Let’s prioritize getting services to people and communities most in need. Let’s protect ourselves, our families, our community. There’s only one enemy: a virus. White House divisiveness is the best ally the novel coronavirus could possibly have.
Now, the disheartening numbers. Detected cases are up three times more than testing. Testing is up 8.6%, while cases are up 24%. What’s more, test positivity has risen from 6.6% to 7.1%. Saying cases are up because of more testing is like saying gravity isn’t real. This is an informative, though depressing graphic from The Covid Tracking Project.
Here’s a good way to show that cases are increasing much faster than testing by state. Case growth has been much higher than test increases in all states. (The published data from Mississippi has been whipsawing.)
Reported cases fluctuate by day. Generally, see lower case numbers over the weekend because of fewer office visits and tests. The weekends are time off for many people, but not for the virus. Paying attention to the seven-day average of reported cases is more useful.
Hospitalizations are, of course, increasing following case increases. It’s shameful and inexcusable that the federal government is not publishing data it has on the pandemic. NPR obtained a recent daily report from the US Department of Health and Human Services, and here’s a screenshot showing hospitalizations increasing:
Will deaths increase? Does night follow day? Of course. We ardently hope that deaths won’t increase as much as in the past, due to better care, fewer overwhelmed hospitals, and the use of dexamethasone and possibly other treatments. But only time will tell. Deaths follow case increases by about three weeks.
Wisconsin is a bellwether … including for Covid deaths. The state has seen a huge increase in Covid deaths. Many other states, sadly, aren’t far behind.
As an epidemiologist, I think a lot about numbers. This week, two numbers made a big impact on me: 13 and 9.
● 13 is the number of years of life lost on average for each of the 230,000+ Americans killed by Covid.
● 9 is the number of people, on average, grieving for each of those deaths.
These represent millions of tragedies, most of the preventable.
We public health specialists must never underestimate the health and social impact of economic harm. We’re heading into a dark winter. We can limit harm with more outdoor activities, open schools, social connections, and shopping. And by reducing indoor maskless contact in poorly ventilated spaces.
I’ve shared some bad news so far. Here’s some good news. 9 of 10 people understand the importance of masking up. Those who don’t are a small, misguided minority. Masking up correlates well with lower case counts. Mask mandates, if done well, boost mask use and save lives.
The increase in telemedicine is also good news. Primary care is the most important part of our health care system, but it’s also the most underfunded and neglected. If we get regulation and reimbursement right, telemedicine will be an important part of fixing primary care and our health care system.
An interesting data survey summarized by Covid Exit Strategy shows that in states with more than 90% mask wearing, less than 20% of people know someone who is sick. In states with 80% or less mask wearing, 30-54% know someone who is sick. Look at the top and bottom places here—the gap is striking!
One of the many, many failures of this administration’s response to Covid has been insufficient protective equipment for health care workers. It makes me SO ANGRY. We’re sending our troops into battle without the armor a competent government would have provided.
Case increases lead to a vicious cycle: longer test turnaround, overwhelmed public health, less isolation of infected patients, more cases. If we reduce cases by wearing masks, watching our distance, washing our hands, and avoiding risky indoor spaces, we can create a virtuous cycle: fewer cases, better contact tracing, and enhanced ability to stop spread.
Why harrowing holidays? Thanksgiving in Canada. The country has struggled with case increases, division, attempts to undermine science, and denials of reality. Even countries which have done relatively well are now struggling. The US, with a completely failed federal response, faces potential devastation.
“Ending the COVID-19 pandemic”? The claim in this White House letter is Orwellian.
The reality is the pandemic won’t end anytime soon. But maybe, soon, there will be an end to the completely dysfunctional national response.0 LIKES SHARE
It’s been a bad week in the fight against Covid. We’ve seen reopenings without sufficient care. Failure by infected people to isolate. Failure to communicate consistently, effectively, respectfully, empathically. A dangerously misguided theory on immunity. Throughout the country, cases are increasing. This will inevitably be followed by increased hospitalizations, and then by increasing death rates.
Test positivity increased for the first time in a month (to 5.4%), but positivity is now more difficult to interpret due to new antigen tests and a lack of consistent definitions and reporting. Hospitalization data is concerning, though in the crazy world of US health economics supply creates demand.
In the past two weeks, 21 states reported their highest Covid rates ever, including in most of the Midwest and much of the West. As predicted, we’ve surpassed 50,000 reported cases per day. The White House cluster is up to 40 known cases and hundreds remain untested. Only two states—Maine and Vermont—are still encouraging.
More information on long-haulers is emerging. We must better understand and care for people who are suffering from the persistent effects of Covid for months after their infection. This excellent article by the incomparable Jane Brody lays out what we know and what we’re trying to find out.
Some people have shamefully misrepresented a recent CDC study which found restaurants, bars, and close contact with Covid patients associated with illness. It’s infuriating to see this kind of misrepresentation, and it’s on par with Wakefield’s fraud on vaccines.
Here’s some great new data on self-reported mask-wearing. More masks → less illness. Masks are a low-cost, effective way to reduce spread.
No place where more than 90% of people said they regularly wear masks had more than 20% of people say they know someone who’s sick. On the other hand, no place where less than 85% of people said they regularly wear masks had less than 20% say they know someone who’s sick. How in the world did masks become political? They’re only against a virus, not a party or person. There’s only one enemy here, and that enemy is the virus that causes Covid.
Three pieces of bad news from this past week:
Remdesivir doesn’t appear to reduce death.
The US continues to fail at contact and source case tracing. This is complex, important, high-skill, high-empathy work.
The dangerously misguided concept of herd immunity through natural infection is spreading.
The reality is that we’re all connected. Infections in healthy people lead to infections in others. “Protecting the vulnerable” requires reducing the risk of infection in everyone. Although the more people who are immune, the slower virus spreads, every infection is a setback, not a step forward. This is not a complicated idea: The way to protect the vulnerable is to have fewer infections, not more infections.
Now three pieces of good news:
At least 199 out of 200 people with the infection recover. Covid is NOT the zombie apocalypse.
Dexamethasone and other steroids—cheap, available meds—reduce the likelihood of death by as much as a third.
Lots of safer social and economic activity is possible.
With Halloween and Thanksgiving coming, we CAN have some safer connections. I shared some ideas on how Halloween can happen without increasing the spread of Covid. For Thanksgiving, I’d suggest that all family members adhere to a strict two week quarantine before any get-together, and only plan to gather if travel can be done safely. That’s what my family is doing.
Let’s not get ahead of ourselves on vaccines. They are our best tool, but just one of many. We don’t know if they will be effective, safe, accessible, trusted. We don’t know how well they will work, how safe they will be, and for how long they will protect people. And even if they are safe, effective, accessible, and trusted, they won’t end the pandemic, and rare, serious adverse reactions may occur. Even if only 1 in a million people, or 1 in 100,000 people have a bad reaction, that’s a lot of people for a vaccine which billions of people may take. It’s always better to underpromise and overdeliver.
Simple measures such as ensuring paid sick leave are also very important. An interesting new analysis found that there was “roughly 1 prevented COVID-19 case per day per 1300 workers who newly gained the option to take up to two weeks of paid sick leave.” This is so important, and would have so many benefits. Should be high on the priority list of all governments.
We in public health must do better understanding and empathizing with the social and economic pain of the pandemic. In the US, there are at least 30 times more people who have lost their job because of the pandemic than have lost their life.
But it’s important to remember, as Ghana President Nana Akufo-Addo said, “We know how to bring the economy back to life. What we do not know is how to bring people back to life.”
Covid is here to stay. We must live fully now, taking steps to protect ourselves and our loved ones.
“The present moment is the only moment available to us, and it is the door to all other moments.” -Thich Nhat Hanh0 LIKES SHARE
The cluster at White House is a symptom and a symbol of the federal government’s failed Covid response. From overconfidence in testing, to lack of basic safety precautions in crowded indoor places, to delayed isolation, incomplete contact tracing, and failure to quarantine, there have been so many preventable missteps.
If there’s one major lesson from this particular failure, it’s that testing doesn’t replace safety measures—testing is only useful as part of a comprehensive strategy. There are often false negatives, and even if a result is accurately negative in the morning, someone could still be highly infectious hours later. That’s why it’s important to reduce risky indoor gatherings and to follow the 3 W’s: wear a mask, watch your distance, wash your hands.
Masks are particularly important. It’s worth reading this edition of our Weekly Science Review by the wonderful Dr. Cyrus Shahpar. I learned from it and was surprised by how suggestive the evidence is. In addition to protecting others and yourself, masks may reduce inoculum and make it more likely that, if you do get infected, you won’t get severely ill.
Rapid isolation reduces secondary cases. There’s strong evidence that paid sick leave reduces the risk that people will work while infectious from the flu, and that is almost certainly the same with Covid. The only valid reason to leave isolation is for a medically necessary procedure.
Contact tracing needs to be done quickly and expertly to find all those who have been exposed to the virus, trace the source of the infection, expand the circle of those warned, and stop the outbreak. Let’s rebrand contact tracing and call it what it is: supporting people who got Covid and who were exposed to it. Instead of “case investigator,” why not “patient support specialist”? And instead of “contact tracer,” how about Covid prevention specialist?
Quarantine means not exposing others after you’ve been exposed. Testing negative is not a get-out-of-quarantine-free card—you can be infectious soon after a negative test. But we should be able to optimize quarantine conditions (a walk outside not near others?) and duration (some places exploring shorter quarantines, with rigorous safety measures after 8 or 10 days) based on data.
Here’s the epi curve of the White House outbreak from what has been publicly reported so far. The pattern strongly suggests common exposure on September 26 or 27. An investigation should be able to determine the likely source and identify those most at risk. And of course it’s possible to identify the source of the outbreak—it just requires wanting to and having the expertise.
The White House cluster isn’t over. There are likely to be other cases. Check out this great graphic from Cleveland Clinic. We need a series of measures to reduce risk, prevent illness and death, and accelerate economic recovery. I’ve been calling it a “comprehensive approach,” but does anyone have a better term?
Controlling Covid requires a one-two punch. In addition to practicing safety measures such as reducing indoor gatherings and the 3Ws, we have to do better boxing the virus in after a new case is identified. We do this through rapid isolation, complete contact tracing, and supportive quarantine. That’s the way we prevent cases from becoming clusters and clusters from becoming outbreaks.
In the US, hospitalizations and deaths are slowly trending downward, but that won’t last because cases are steady or increasing in most of the country. Only Maine and Vermont are reassuring. Unfortunately, there will be continued increases in cases, and eventually deaths. There will be 230,000 reported deaths by November 3. A sobering number. We have one of the highest cumulative death rates of all wealthy countries.
In New York City, we’re continuing to see uncontrolled spread in religious communities and increasing risk elsewhere. Note that this is the same community that had extensive spread in the spring - so hopes that a low level of infection will lead to herd immunity are false, and dangerous (more on this next week). The ONLY way to stop spread in this community is to engage the community, support and collaborate on education from within, and encourage religious leaders to establish and manage acceptable isolation facilities.
Some good news is that schools, if run well, don’t appear to be major amplification points for the virus. At Resolve to Save Lives, we’ve been saying since March that we must keep in-person learning as available as possible, which means reducing spread in the community and adapting the school environment and policies.
As the late New York Senator Daniel Patrick Moynihan said, “You’re entitled to your own opinion, but not your own facts.” And to quote epidemiologist William Farr, “The death rate is a fact; anything beyond this is an inference.” The cumulative US death rate has now passed the UK, approaching Spain, highest of high-income countries. Read the graph, and weep.
We cannot become hardened to horror of continuing, preventable Covid deaths. Every life is precious. Who saves a life, saves a world.1 LIKES SHARE
Although there have been 7.4 million reported infections in the United States with the virus that causes Covid, estimates suggest that the number of actual infections is about 40 million, at least. The infection of President Trump is the most prominent, and one of the most telling.
My thoughts are with the President, First Lady, their family, and all others infected with and affected by Covid. The President’s infection is a reminder that Covid is an ongoing threat. No one is safe – not even heads of state – until everyone is safe.
Risk of severe illness and death increases steadily with age. A 74-year-old has approximately a 3% chance of death. Once it became clear that he had symptoms, the estimated risk increased to about 10%. If he had a clear indication for hospitalization (moving him to Walter Reed was clearly the responsible thing to do, whether or not he had an indication for hospitalization), the risk could be as high as 25%. The risk is even higher in males than females, and higher in people who are obese, and lower with good care. 85-90% of those infected in their 70’s will have no, mild, or minor illness. Of those with symptoms in this age group, 90% recover.
People who get prompt medical care, including oxygen, likely have better outcomes. Remdesivir may reduce the duration of illness. The data on convalescent plasma is contradictory. Monoclonal antibodies, which the president received, are promising (especially early in illness) but unproven. Dexamethasone, which the president also received, may reduce the risk of death by about a third, but is generally thought to be most helpful late in the course of illness, when a patient’s own immune system, rather than the virus, is causing much of the harm.
Testing is only useful as part of a comprehensive strategy. What’s important isn’t how many people are tested or how often, but what is done with testing to reduce risk. Testing doesn’t replace wearing a mask, watching your distance from other people, and washing your hands.
It’s a plain truth that face masks protect others, and almost certainly protect yourself as well. The more people who wear masks when we’re near others, the safer we’ll all be. Did the extensive testing done at the White House give a false sense of security? Absolutely.
We need to rebrand contact tracing. Let’s call it what it is: supporting people who have Covid and those who were exposed to it. Could Vice President Biden and Chris Wallace be at some risk from the debate? Maybe. The louder someone talks, the greater chance the virus will spread.
Every person infected with Covid is a step backwards in our effort to slow the pandemic and reopen society. We’re nowhere near herd immunity, and getting there without a vaccine would cost hundreds of thousands of lives and millions of jobs.
We must better prevent and treat this virus. We’re all in this together, and the better we prevent and fight it, the more lives we can save, and the sooner and safer we can get to the new normal.
Overall in the US, most states had increases in Covid spread during the month of September.
The new trend feature on Covid Exit Strategy is helpful, although the trends are discouraging.
The only states with reassuringly low rates of Covid are Maine, Vermont, New Hampshire, and perhaps Connecticut. Many states, such as Florida, are opening despite persistently high positivity rates, and will inevitably have further increases in the coming weeks. These actions raise the question: is this action, which will increase cases in a month, intentional or just neglect of science?
Closer to (my) home, NYC is on the edge of a precipice. We’re seeing extensive and ongoing spread in religious communities and likely beyond, meaning there’s a very high risk of a resurgence. Here are the positivity rates in hotspots, according to Governor Cuomo (Media statements from the city government have shockingly lacked basic information on the number of people tested and positive cases, as well as on trends).
For more than a month, NYC has had 300 or so diagnosed cases a day, but we still lack basic information about how the city is doing. We need to know:
What proportion previously identified as contacts and were in quarantine already?
For how many was the source identified?
Average time from symptom onset, or test taking, to isolation?
Are cases isolating? Contacts quarantining?
It’s challenging to work with a religious community that doesn’t trust the government. How about hiring 1,000 people from the community through acceptable intermediary organizations to fight Covid? The key is to start ASAP, standardize training and performance monitoring, and get community buy-in.
Gandhi’s birthday was Friday. I think about his call to empathy and to recognize that our enemy is hatred. We’re all connected. Unless we work together to fight Covid, the virus will continue to have the upper hand.
0 LIKES SHARE
(Original article published on Tom Frieden’s LinkedIn account https://www.linkedin.com/pulse/covid-week-virus-strikes-back-tom-frieden/)
People are tired of fighting the virus, but the virus isn’t tired of infecting people. As parts of Europe and the US show, if you turn your back on Covid, it will come back to bite you. Cases are trending up again in many states, and are likely to hit 50,000 a day in the US in October.
Trends in positivity are hard to track, and getting even harder to track. Per the Covid Tracking Project, only 9 states currently followthe best practice of reporting antigen and PCR tests separately. States should also report the proportion of unduplicated people who tested positive, cross-referencing the two types of test.
What starts in the young doesn’t stay in the young. The MMWR reports that young adult infections were followed a week or two later by infections in people over 60. We’re all connected. The sooner we recognize that, the sooner we can move forward more safely.
These are some of the top Covid hotspots.
Universities
Meatpacking factories
Jails, prisons
Homeless shelters
Meatpacking factories are driving spread in many communities, with persistent failures in prevention, response, and transparency. It’s crucial that we take action to stop spread in hotspots.
Covid is spread by particles – some large, some small. It's a continuum, not a dichotomy. In crowded indoor spaces, Covid can spread widely, but it’s much less infectious than measles. Measles commonly spreads through air that can stay contaminated for hours -- for example, people in an emergency department can get infected hours after a patient with measles has left. This is likely much less common with Covid than with measles. Transmission depends on the index case, ventilation, whether people are wearing masks, what activities they’re doing (singing, shouting, etc.), and who is exposed.
Recent spread in Orthodox areas of NYC is concerning. Given crowding and alienation from government, spread within the community is a near-inevitability, but wider spread in NYC can be prevented if the city does much better at rapid isolation and effective contact tracing.
For eight months, the US government has ignored, sidelined, and undermined public health and scientific recommendations. They have taken the tools we have to fight Covid and broken them. Masks. Testing. Effective communication. Contact tracing. Strategic closures. Careful reopening. These are all things we should be doing better.
Operation Warp Speed, the effort to deliver a Covid vaccine, has gotten some things right. For example, they’re testing multiple vaccine candidates, manufacturing in parallel with studies, and providing good CDC guidance on vaccine preparation. But if vaccine studies are stopped early, we’ll lose essential information on effectiveness in the elderly and safety for all.
Vaccines are our most important tool in the fight against Covid. We can only hope the administration doesn’t break this tool as well by meddling with the science and the approval process. Errors by the administration have already cost lives and jobs. Politicizing vaccination would be the most dangerous and costly mistake yet.0 LIKES SHARE
(Blog initially published on Tom Frieden’s LinkedIn account: https://www.linkedin.com/pulse/covid-epi-weekly-one-step-forward-back-tom-frieden/)
We’re seeing decreases in Covid cases and test positivity rates in much of the country. That’s good news. But there’s also been less testing, less information about how the virus is spreading, and impending explosions with schools and universities reopening.
“A single death is a tragedy, a million deaths is a statistic.” My primary concern is that people may become desensitized to the sheer number of deaths caused by the pandemic. Close to 200,000 people have been killed in the U.S. That’s staggering.
The positivity rate decreased from 5.5 to 5.1% nationally, which is progress. But we’re losing the ability to track the virus—new antigen tests are difficult to track, there’s been less testing overall, and there’s still no reliable information on who is being tested. We should be getting better information each week, but we aren’t.
Most of the US is still failing to contain Covid. There are too many cases to test, trace, isolate. Even in places with fewer cases, there’s very little tracking of actual outcomes of testing and contact tracing. We need to know the average number of days someone is infectious before isolation and the percentage of cases arising from among quarantined contacts. Tens of thousands of lives and millions of jobs depend on this.
It’s outrageous that we STILL don’t have reliable information on cases, hospitalizations, and deaths by week by race and ethnicity. Every place should report these numbers weekly. The disproportionate impact on Latinx and Black communities unacceptably high and indefensibly invisible.
Avoidable cases and deaths are heartbreaking. Avoidable economic decline is grinding. James Carville famously said, “It’s the economy, stupid!” Well, to get the economy back, “It’s the pandemic, stupid”. Unless we control the virus, we can’t get our jobs back.
Deaths matter most. The US will hit 200,000 deaths and the world will hit 1 million reported deaths in the next few weeks. Germany has had less than one-fifth the US death rate, Canada less than half, and South Korea 80 times less. Tens of thousands didn’t need to die from Covid. We certainly don’t want to be #1 in death.
On 9/11, I reflected on deaths. My group is called Resolve to Save Lives for a reason. But we risk getting hardened to tragedy. Ed Yong wrote a superb article on this phenomenon and more in The Atlantic. More than 1,000 Americans a day have died recently from Covid. Even at “only” 500 deaths a day in the U.S. this would represent:
More than all injuries
1.5x all Alzheimer’s deaths
2.2x all diabetes deaths
3x all overdoses
4x all suicide deaths
9x all homicides
32x all HIV deaths
In fighting the pandemic, communication matters. If the goal is to prevent panic and save lives, there’s a proven way of doing it: 1. Be first. 2. Be right. 3. Be credible. 4. Be empathetic. 5. Give people practical things to do to protect themselves, their family, and their community. Is it possible for the US national response to have violated these principles more than it did?
We can control Covid, but to do so we must chip away at it. Close the riskiest places. Mask up. Box the virus in (test, isolate, trace, quarantine). Improve ventilation. Every little bit can help, as long as there are a lot of little bits to get R<1 and keep it there. Vaccination can help if it's safe, effective, accessible, and trusted. IF.1 LIKES SHARE
(Blog initially published on Tom Frieden’s LinkedIn account: https://www.linkedin.com/pulse/message-young-people-from-public-health-doctor-tom-frieden/)
Young people are facing a lot of stress and uncertainty right now. Schools in many places are closing almost as soon as they reopen. Sports, concerts, and large gatherings are a no-go. Recent college grads are entering a flagging economy.
I received a note the other day from an 18-year-old high school senior who's concerned and feels he may be getting depressed about the future. He asked when he'll be able to attend a sports game or concert again, when he'll be able to visit his grandparents, and if we'll ever get back to normal life. He asked, Will this be forever? Are we doomed?
Anyone who’s definitive about certain things about Covid simply doesn’t know enough about Covid. This is a new virus. It’s spent less than a year living with humans and we’re learning more every day. It's helpful to address what we know right now and with what level of certainty.
Here are a few things we know, and my best take on our level of certainty:
The virus can be deadly, particularly for older people, for some people with underlying health conditions, and, more rarely, for the unlucky people who get very sick or die even without underlying conditions. About this, we are 100% certain.
Wearing a mask protects people around you, particularly if you wear it correctly, and particularly in indoor environments. About this, we are also basically 100% certain. That doesn’t mean masks are 100% protective, it just means that wearing a mask reduces the risk to others.
Wearing a mask may protect you from getting infected, and may possibly protect you from becoming very ill if you do get infected. This is likely, but not certain, and depends in part on what kind of mask you wear and whether you put it on, wear it, and take it off correctly.
People who have gotten very sick from the virus appear to make antibodies, including neutralizing antibodies. This is 100% certain.
Antibodies, particularly neutralizing antibodies, may protect at least some people who have recovered for at least some time against getting infected with Covid again. We hope this is true, but it is not yet proven. Many of us (myself included) think it is the case, but how well these antibodies protect, and for how long—or even if they protect at all—isn’t known. I wrote about the perils and promise of immunity here.
A vaccine that is safe and effective may become available by early 2021. Many people hope this is the case, but we will only know when studies are done.
Now, what does all that mean for the question about whether this will be forever?
First, I would assume that for the next year (at least) masks are going to be important, particularly when indoors and when there are many people in a space that isn’t well ventilated.
Second, I would also assume that, even if we have a vaccine, we’re going to need to adapt our lives in certain ways for at least a few years. That’s because a vaccine isn’t likely to be perfect, nor are 100% of people likely to take it. That doesn’t mean we won’t be able to get much of our former lives back, but it does mean there are likely to be some differences. I shared why we have to accept a new normal and the possible hurdles and limitations of a vaccine. My mother is 91 years old and used to love to sing in chorus, but there’s no way she can go back to doing that any time soon.
So, will we be able to go to an indoor concert safely in 2021? We don’t know. Germany just did a fascinating experiment. They had an indoor concert with everyone wearing masks, but repeated it 3 times—with distancing, with some distancing, and without distancing. We may learn from that.
Will we be able to go to sporting events in 2021? Outside, definitely. Inside—same as the concert, we don’t know. (We do know that the louder people shout or sing, the more they can spread the virus, though much less so if they’re wearing a mask.)
Will we be able to go to indoor concerts and indoor sporting events safely in the next few years? I think yes. By then, we’ll almost certainly have a safe and effective vaccine, and we’ll certainly have better treatment. And I hope we’ll have a better public health system so that we can quickly test, trace, isolate, and quarantine so that when there are cases they don’t become clusters, and clusters don’t become outbreaks.
I don’t think masking will be forever, but I do think there will be some changes in how we go about our lives for the foreseeable future. Handshakes are probably out for a while. We should learn from Asia and wear a mask if we don’t feel well—or, better yet, stay home.
There’s actually an article about how to hug grandparents and other elderly loved ones more safely. And what my brothers and I do is to quarantine for 14 days before we see our mother, and maximize time outside together when we do see her.
We’re definitely not doomed. We—especially young and thoughtful people—have enormous potential to control our future. Even without a vaccine or treatment, communities in countries around the world have stopped the spread of the virus and gone back to life almost as before. With a vaccine and treatment, even more progress will be possible. Ironically, to get our individual freedom back, we need to work together.0 LIKES SHARE
(Blog initially published on Tom Frieden’s LinkedIn account https://www.linkedin.com/pulse/united-states-both-stalling-failing-our-effort-combat-tom-frieden/)
September 5, 2020. Continued spread of Covid in the US will continue to undermine health, jobs, economy, and education. A concerted, strategic approach would help, a lot. Parts of the Federal government are making a fundamental error: Failure to recognize we’re all connected, all in this together. Spread in any place or group is a risk everywhere, and if we work together, mask up, increase distance, improve testing, tracing, and support for patients and contacts, we can get more of our economy, more of our jobs, and more in-person education back.
Some are speaking about this outbreak as if it’s in the past tense. But more than 4 out of 5 Americans aren’t yet infected - it could get a lot worse, and it will if we don't improve our approach.
According to CDC’s CovidView, test positivity inched up from 5.4 to 5.5% in the past week, driven by an increase in positivity among 19-49-year-olds (and this is before many colleges try to open). Test positivity is at low levels in the northeast and some other states, but very few places are finding where most spread is occurring - most sources of infection, and even fewer -- maybe none -- are quarantining most contacts effectively. Because of that, virtually everywhere, the risk of explosive outbreaks remains. Rates of infection and of test positivity are high or increasing rates in most of the US. These rates are too high for economic and social recovery.
There are two data sources of note. County-specific test positivity, which should be open source but at least is available here (image below -- I wish they had zip code lookup).
And we’re delighted to work on the Covid Symptom Data Challenge. This could become an important early warning system for Covid. The competition is open until September 29.
Deaths and hospitalizations continue to decrease overall. But 500-1,000 deaths/day is horrific. These deaths also reflect approximately a quarter of a million infections per day a month ago (so we’ve only been detecting about 1 in 5 infections).
There were 215,000 more US deaths March-July than baseline. Of these, 71% were diagnosed as Covid by their doctor. The remainder were either undiagnosed Covid or deaths from Covid-disrupted care. Covid-disrupted care is an even greater risk in Africa and elsewhere, where measles, malaria, and other causes of death can rapidly and drastically increase death rates. Good tracker by The Economist.
Imagine how many fewer deaths the US could have had if the Federal government had focused right. One example: masks vs. hydroxychloroquine. Masks work. Places around the world that used masks consistently had half to two thirds less spread. 100,000+ deaths could quite possibly, simply, and cheaply have been prevented.
Good news on steroids. Confirmation that they help with severe Covid. The sicker you are, the more they help, with up to a 35% reduction in risk of death in the sickest patients. Yes, really, 35%. Nice review of all key data by WHO. Yes, really, WHO. Press conference, anyone?
I’m guardedly optimistic that we’ll have evidence of a safe and effective vaccine in the next few months. But we need to look at all the data. Efficacy is more likely to be proven early than safety. So when one CEO spoke recently of having early data because there are lots of events, that’s a big concern, because the events he’s talking about are Covid infections in trial participants who got placebo. We need transparency about what safety signals are being looked at. There are at least two important concerns about safety:
Inflammatory reactions. MIS-C in children - the Kawasaki-like syndrome - is the result of immune over-reaction. Will this happen with a small proportion of people vaccinated? How will we know? What sample size is needed to evaluate for this?
Antibody-dependent enhancement. This means that infection with the virus that causes Covid after vaccination could, for some people, result in more serious illness. This occurred in one animal model, for one vaccine against SARS. How is this being evaluated for? What is the sample size needed?
Oh, and for the mRNA vaccines, what adverse events do we even look for? We've never used this type of vaccine in people before.
Lots has been done right with Operation Warp Speed (multiple vaccine types, manufacturing and trials in parallel), but let’s hope they don’t warp the science. There’s no way to stop epidemics without trust. Politicizing data and decisions is essential for trust, and very, very dangerous.
The pandemic ain’t over until it’s over, and it’s nowhere near over. Even with a safe, effective, available, and trusted vaccine, it would be months or years before the risk of deadly outbreaks is down to manageable levels. We need continuous improvement in testing, isolation, tracing, and quarantine. The 3W’s make a big difference: Wear a mask, Watch distance, Wash hands. Improving ventilation and spending more time outdoors also help. Smarter limitations on activity can balance jobs and health. We’ll need to make preparations for vaccination, hoping that safe and effective vaccines become available. These including improving the cold chain and engaging communities. It's past time to begin conversations with communities, sharing what we know and don’t know and listening to concerns and perceptions.
Cases in the United States remain at a high level, increasing in much of the country, and we continue to fail to implement an effective, coordinated response.0 LIKES SHARE
(Blog initially published in Tom Frieden’s LinkedIn account https://www.linkedin.com/pulse/covid-week-decreasing-cases-increasing-danger-tom-frieden/)
The latest data show that Covid is decreasing from very high levels to high levels in much of the U.S., but don’t be lulled into a false sense of security—danger is still very present. Schools are reopening and outbreaks are inevitable. And although human immunity against the virus now appears possible, FDA and CDC immunity from political interference is much less so.
First, the trends from last week. National test positivity decreased from 6.2 to 5.7%, which confirms that there has been a steady decrease in cases over the past few weeks. Case rates in the Northeast remain relatively low, and these states are now joined by MI, WV, NM, MT, WY, AK which have relatively low rates. The number of tests done decreased in some states, including Florida. Antigen testing—which is much faster than most PCR testing but less reliable—will make the national positivity number harder to track, and there’s a risk that many antigen tests won’t get reported. State and local health departments need to receive 100% reporting of PCR and antigen tests.
To date, the US has seen more than 500,000 cumulative hospitalizations, 6 million diagnosed cases, 180,000 reported deaths, plus at least another 50,000 or so excess deaths above baseline, which are from a combination of undiagnosed Covid and Covid-disrupted care. To put the U.S. situation into perspective, the US Covid death rate just for last week was more than three times the rate in South Korea since January.
The Latinx population in the U.S. as well as many Latin American countries are being very hard hit by the virus. Many are essential workers who have insufficient protection, are more likely to face crowding, have lack of access to care, and have underlying health problems. Peru now has the highest cumulative death rate in the world, and also has many unreported deaths.
There are high hospitalization rates in Native American, Latinx, and Black communities in the U.S., but these numbers are gradually declining. We can only reopen more by staying safer, masking up, and finding and stopping spread with the box-it-in strategy.
Masks matter. At Resolve to Save Lives, we released a toolkit this week sharing evidence, tools, and best practices for policymakers and communities to promote mask-wearing, which I summarized in the Washington Post. Masks are one of the lowest-cost, most effective tools we have to get more of our economy, education, and health care back. Mask up to keep deaths down. Kudos to Philadelphia for measuring and improving use. 
These are troubling times, not just because of epidemiological trends but also because of political interference with science. It’s been said that in war, truth is the first casualty. In this war against a virus, truth can be our strongest weapon.
Indefensible framing by the FDA of emergency use authorization (EUA) for convalescent plasma threatens to undermine trust in the agency. Convalescent plasma is a 100-year old treatment that may work, a bit, for some patients. There’s still so much we don’t know. For example: What antibodies should be used? For which patients? When in the course of illness? What dose? For how long? We need more science and less politics.
The CDC also made an indefensible recommendation, dictated by White House/HHS, that asymptomatic contacts of Covid-positive patients don’t need to be tested. That recommendation is not backed by science. We need to test asymptomatic contacts. If these contacts are positive, their contacts can be identified, warned, and quarantined. Not testing asymptomatic contacts allows Covid to spread. Let’s hope the CDC website gets corrected.
There have been far too many preventable casualties from the failed US response to the pandemic already: lives, jobs, education, and more. We cannot let the FDA and CDC become the next casualties of Covid. We must base decisions on science and insist on complete transparency on data and process.0 LIKES SHARE
(Blog initially published in Tom Frieden’s LinkedIn account : https://www.linkedin.com/pulse/dozen-observations-covid-19-immunity-tom-frieden/)
Immunity is tricky. We think of it like armor – if we’re immune, we’re protected. But it’s much more complicated. Every day, we learn more about immunity to SARS-CoV-2, the virus that causes COVID-19. On balance, what we’ve learned is good news, but there are important caveats and implications.
First, the good news:
1. Recent laboratory studies suggest – but don’t prove – that immunity from infection with SARS may last many years.
2. These same studies suggest that antibodies, which have been a focus of research, may not be the only, or even the most important component of our immune response.
3. Animal studies suggest that infection protects against re-infection, at least in these animals, at least in a laboratory model, at least for a few weeks.
4. A small but interesting study suggests that neutralizing antibodies in people may be protective against re-infection, at least for some time for some people. It’s not enough to bet your life on, but it’s enough to be optimistic about the potential for immunity.
Now, the caveats:
1. We don’t know how long immunity, if it occurs, will last or how complete the protection is. Overconfidence could lead individuals and communities to let their guard down, which could result in more spread and more death. Testing positive for antibodies does NOT mean you’re immune.
2. We don’t know what proportion of people with natural infection will become immune.
3. We don’t know if some people who get vaccinated will develop harmful immune over-reaction.
4. Even if 20% of the US population has been infected, we’re nowhere near herd immunity. Not all infected are necessarily immune, and, more importantly herd immunity likely requires at least 60% infection rates, and in any case isn’t an on-off phenomenon. When more people are immune, infection spreads more slowly. But because spread is uneven, communities remain vulnerable even if a high proportion of the population has been infected. Getting to herd immunity in the US would require hundreds of millions of infections and at least a million more deaths. That’s not a plan, that’s a catastrophe.
And now, the implications:
1. The likelihood that an effective vaccine will be found is increasing. Why? Because Mother Nature usually does better than our best vaccines, and the ceiling of vaccine efficacy is usually protection after natural infection. But vaccination won’t be quick or simple. We have to ensure it’s safe, effective, available, and trusted.
2. We need to be particularly careful about vaccine safety. Developing immunity — either through infection or vaccination — may result in severe illness. This is why some people get so sick with COVID-19, and likely why dexamethasone, a medication that weakens the immune system, helps some severely ill patients. It’s a concern with vaccination, which could potentially harm a small proportion of patients because of immune over-reaction – either from the vaccination itself, or from exposure to the virus after vaccine-induced immunity. This is being studied in the vaccines being developed and will need to be tracked whenever they are given.
3. It’s possible, once vaccination is widely available, that immunity passports – certificates of immunization (or, potentially, of protective immunity from infection) will become a reality. This is already done (not well) for Yellow Fever. If it helps us reclaim our education, jobs, and economy, this could be a good thing – but there are important risks to be considered. (We outlined some controversies: “…perverse incentives, muddled risk communication messages, violations of patient privacy, diversion of resources, fraudulent certificates, and creation and perpetuation of inequalities, among others.”)
4. We can get to a new normal if we improve control today, stay apart, work together, and prepare for vaccination if and when it becomes available. For now, we need to continue to wear masks, watch our distance, and wash our hands. Our schools and universities need to be extraordinarily careful. In most of the country, we need to keep our bars closed, indoor dining closed, and avoid closed indoor spaces with lots of people present. There may be light at the end of the tunnel, but immunity is definitely not just around the corner!
There’s still more we DON’T know than what we do know about immunity to the new coronavirus. Humility remains very much in order. Learn, share knowledge, discover, move forward carefully, guided by science and a focus on protecting both lives and livelihoods.1 LIKES SHARE
Here’s where we are in the US with Covid now. This is based on CDC’s latest COVIDView report, Covid Exit Strategy and other sources.
Outbreaks in the US have gotten so bad, the folks at Covid Exit Strategy added a “bruised red” to their map, signifying states where the virus is out of control. The bruise is spreading.
In the past week, overall test positivity increased slightly, although positivity in commercial labs decreased slightly. Something odd is going on with the commercial lab data—the number of tests reported is way down and we’ll have to wait until next week to know if these trends are reliable.

Look carefully at the public health lab results. Lines are positivity rates, on the Y axis. Note the yellow—young adults—increasing for more than a month. Older adults (blue and green lines) increased sharply last week. That’s not good. Because there’s a lag in deaths we’ll first see an increase in cases. The deaths follow 2-3 weeks later.

Test positivity trends are revealing, but don’t be fooled by test numbers. I don't know why people are wondering if we will have more than 100,000 infections a day in the US. On Saturday there were at least 200,000, possibly many more than that. We diagnose only a small fraction.
Many tests take more than 2-3 days to come back, which means they are of little value. We should know testing rates for each race/ethnic group and ensure all results come back within 48 hours.
Influenza-like and Covid-like illnesses are continuing to increase in much of the country. This syndromic surveillance is an important early warning system that first sounded the alarm in Arizona in late May…
Death rates have declined to near baseline. Hans Rosling got it right: we have a hard time conceptualizing that a situation can be better, but still very bad. We’ve seen a dramatic increase in the use of Remdesivir and a steady increase in plasma treatment in hospitalized patients with Covid. These are promising though unproven treatments.
Here are the most alarming states, with high rates of Covid and high and rising test positivity: Florida, Texas, Georgia, Louisiana, South Carolina, Alabama, Nevada, and Idaho.
Arizona has stabilized at a high rate. California, Utah, and many other states are seeing intermediate levels of spread; the population of California means large numbers of cases there.
Reassuring so far, but still at risk: Northeast, Wyoming, South Dakota. Hawaii and Alaska have low rates with small increases.
Where does the epidemic go from here? This modeling site has performed better than most, using solely deaths and machine learning. Nationally, Youyang Gu estimates there are 4.8 million people with Covid today—1 of every 78 people.
The same site projects 211,500 deaths in the US by the end of October. Leaving Belgium (which counts deaths differently) aside, that would put the US death rate ahead of France, Sweden, Italy, and Spain and about tied with the UK for worst in the world.
Better care and newer treatment can decrease death rates (maybe: plasma and remdesivir early, steroids for some patients late). Even with a vaccine, the virus is here to stay. We need a comprehensive response that will minimize deaths and get to the new normal soon and as safely as possible.
There’s a lot at stake. The chance for our kids to go back to school and for us to get back to work. The chance for our economy to recover. The chance for us to save tens of thousands of lives.
Stay tuned for news Tuesday about a better way to get a nationwide approach despite lack of national leadership.
It’s not about opening schools or our economy, it’s about opening them and keeping them open. We know what to do: follow the 3 W’s—wear a mask, wash your hands, watch your distance (e.g., close restaurants and bars), and box the virus in with strategic testing, isolation, tracing, quarantine.5 LIKES SHARE
(Blog initially published on my LinkedIn profile https://www.linkedin.com/pulse/latest-covidview-us-lagging-control-surging-cases-tom-frieden/)
Here’s where we are in the US with Covid now. This is based on CDC’s latest COVIDView report, Covid Exit Strategy and other sources.
It’s clear the US does not have COVID-19 under control. Virus is surging, and our response remains fragmented. Only the Northeast is at all reassuring, and those gains are at risk. Reopening schools and restoring our economy are getting much harder.

Test positivity across the US is up to 9.2%. The South Central region is at 17%! See the interesting trends from commercial labs in this graph below. It shows the first decrease in positivity among young adults in 2 months...and now positivity is increasing in older adults. As predicted, what started in young adults didn’t stay in young adults.
We should be seeing testing rates by race and ethnicity—and all tests results must come back quickly. Tests that take more than 48 hours to come back are of little value.
Influenza-like and Covid-like illness visits to emergency departments are rising in 7 of 10 US regions.
Native American, Black, Latinx and other communities continue to be disproportionately affected. They’re more exposed, have more underlying conditions and undertreated illnesses, and also have less access to care. Community engagement, empowerment, and leadership is crucial for progress.
Covidview deaths are below the epidemic threshold, but how long will that last? Overall US deaths are now rising.
Deaths are rising most in the South, Southwest, and West, offsetting the decline in New England, Mid-Atlantic, and Midwest. And this is before young adults spread to lots of older and vulnerable people. The next one to two months will be worse, unfortunately.
States with the highest Covid burden are least able to test and trace right now.
The situation will get worse before it gets better. Where Covid is spreading and in most of the US it will be essential to close restaurants and bars, stop gatherings of more than a few people, and box the virus in through strategic testing, effective isolation, rapid contact tracing, and supportive quarantine. We all must follow the 3 W’s—wear a mask, wash your hands, watch your distance.
Otherwise, there’s little hope of safely opening schools, no matter what anyone says.0 LIKES SHARE
(This blog was originally shared on my LinkedIn account: https://www.linkedin.com/pulse/where-we-covid-19-pandemic-good-bad-week-tom-frieden/?trackingId=GnuqPnY5Q26fXQu2W8YIWg%3D%3D)
Another momentous and painful week. With it, another CDC COVID-View report. Below is a quick summary of the key findings.
One big thing to note is what’s not reported: case numbers, which are largely irrelevant. We actually find only about 1 in 10 cases, and the numbers are highly dependent on testing intensity and the testing approaches used.
First, the good news on COVID-10 epidemiology. The percentage of positive tests continues to decrease, as do trends for the proportion of outpatient visits for ILI and CLI (influenza-like illness and COVID-like illness). These proportions can be misleading because when people do not go to healthcare facilities or seek treatment to avoid exposure to COVID-19, the proportions can increase even if infections are decreasing. It’s important to track both the proportion and numbers of ILI/CLI.
Now, two pieces of not-so-good news:
First, in 4 regions, the southeast, southcentral, west coast, and pacific northwest, test positivity has increased.
Second, the positivity rate in kids continued to stay stable or increase.
The leading hypothesis is that adults are bringing infection home to their kids. To remedy this, we should offer housing for the infectious period for all with COVID-19. This is what the best programs around the world are doing. This limits spread and protects families. This should, of course, be voluntary and provide appealing, temporary housing.
Race/ethnicity inequalities continue to persist, with Native and Black people having 5x hospitalization rates and Hispanic/Latinx people having 4x the hospitalization rates of white people. This disproportionate burden requires a disproportionate response. We must focus on protection, prevention, engagement, and support.
Now, for the most encouraging trend. Deaths continue to plummet. Within a week or two, death rates may be at or near the baseline IF trends continue. Note, the below chart shows the percent of death from pneumonia, influenza, and COVID-19. We use percent, not number, because this is the most reliable indicator.
But, even with this trend, there could still be hundreds of deaths from COVID-19 each day. It’s preventable. It’s tragic. And it represents continued spread and risk of the virus. However, Europe, which is weeks ahead of us epidemiologically, appears to be reopening without rekindling -- yet.
So, we will wait and see. What should you do? What you have been doing. Wear a mask. Wash your hands. Watch your distance from others. Box the virus in: test, isolate, contact trace, and quarantine. Continue to track the pandemic and our response to it. Importantly, protect nursing homes, the homeless, jails, factories, and anywhere where large numbers of people congregate. Hope for the best, plan for the worst.1 LIKES SHARE
Blog initially published on my LinkedIn profile ( https://www.linkedin.com/pulse/down-covid-19-virus-up-economy-tom-frieden/?published=t )
We all want two things: to get back to work and to as normal a life as possible and to not endanger the health of ourselves, our loved ones, and others. Personally, I can’t wait to get back to the gym. The better we control the virus, the sooner we can restart our economy because to protect livelihoods, we must protect lives. And the quicker we get back to work, the healthier we will be.
Last week, Resolve to Save Lives released a four-level, color-coded alert system for COVID-19 that could be implemented by city, state, and national governments — with wide consultation within society.
This alert system can achieve three objectives:
It empowers people to protect themselves and their families. There are times when older adults and people with serious health conditions should be extra careful to avoid infection. And businesses, schools, health care facilities, nursing homes, and others need practical information on what they can do at different levels of risk.
It holds government – and all of us – accountable.
It can accelerate progress on reducing risk by focusing on crucially important things we can do to restore economic activity and fight the virus without rekindling the pandemic.
By adopting an alert-level approach, we can empower people, hold governments accountable, and accelerate progress. We can recover our economy without risking our lives.0 LIKES SHARE
This blog was originally published on my LinkedIn profile (https://www.linkedin.com/pulse/groundhog-day-congress-time-might-work-tom-frieden/)
On May 6th, I had the opportunity to testify in front of the House Appropriations subcommittee on Labor, Health and Human Services, Education, and Related Agencies to discuss the COVID-19 pandemic.
As CDC Director, I testified many times in Congress, often with the same message: we have to increase and sustain investment in public health systems in the U.S. and globally to keep ourselves safer. Other than wearing a facemask, using a lot of hand sanitizer, and hearing strong support from many in Congress, there was one major difference this time: it might actually happen.
It was surreal to walk through empty halls of Congress and speak in front of masked representatives, but this reflects our new reality.
Tom Frieden testifying in front of the House Appropriations subcommittee on Labor, Health and Human Services, Education, and Related Agencies
Just projecting from the number of people already infected and being infected now, the virus will have killed at least 100,000 people in the U.S. by the end of the month. But we can get through this. It’s us against them – humans against the virus.
There are 10 plain truths we need to accept in order to move forward productively and effectively.
1) It’s really bad.
In New York City, it’s on the order of the influenza pandemic of 1918-1919.
2) As bad as this has been, we’re just at the beginning.
Until we have an effective vaccine, unless something unexpected happens, our viral enemy will be with us for many months or years. There is no magic bullet. Not travel restrictions. Not staying at home. Not testing. Not Remdesivir. All of those can help, but until and unless we have a safe and effective vaccine, there’s no single weapon that will deliver a knock-out punch.
3) We need to be guided by the data.
We need accurate and real-time monitoring to track trends in symptoms, emergency department visits, tests, cases, hospitalizations, deaths, community mobility, and more. We must work to find cases before they become clusters, clusters before they become outbreaks, and outbreaks before they become explosive epidemics that risk the lives of health care workers and others.
4) We will be able to begin to re-open as soon and safely as possible by basing decisions on data and creating a new normal
Sheltering in place is a blunt but effective weapon: it suppresses spread of the virus but inflicts severe hardship on individuals and the economy. After flattening the curve, the next step is to box the virus in by implementing four essential actions – test, isolate, contact trace, and quarantine. All are crucial; if any one is weak, the virus can escape and spread explosively again. If we do all of these four things well, even if we don’t have a vaccine, we can begin to return our society and economy to a more normal footing.
5) We need to find the balance between restarting our economy and letting the virus run rampant
We’re conditioned to think in dichotomies of A vs. B – but open vs. closed isn’t a true dichotomy. We need to think of this more as a dimmer dial than an on-off switch, with different gradations of open based on what we can do without undue risk. Many measures we’re seeing now – floor markings to denote safe distancing, requirements to use hand sanitizer before entering a building, capacity restrictions in restaurants and stores – may be with us for some time.
6) It’s crucially important to protect the health care workers and other essential staff who are the front-line heroes of this war.
They shouldn’t have to put their lives at risk to care for us.
7) We must protect our most vulnerable people.
Nursing homes and other vulnerable congregate settings house approximately 4 million people in the United States. Unless we take urgent action, at least 100,000 residents of America’s nursing homes will die in the next year, and there could potentially be hundreds of thousands of deaths in all congregate facilities, including among those who work in these locations. We must also act urgently to reduce the higher rates of infection and death among African American, Native American, and Hispanic people.
8) We must invest in a vaccine and therapeutics.
Governments and private companies must join forces to make massive, continued investments in testing and distributing a vaccine as soon as possible, ensuring rapid and equitable access in this country and around the world. Nothing else will enable life to get back to a pre-COVID normalcy.
9) We must heighten, not neglect, our focus on non-COVID health issues in order to increase personal and community resilience.
Underlying conditions greatly increase the risk of severe illness. We need to preserve health care services despite the pandemic. We must take steps to avoid people postponing care for strokes and heart attacks, delaying cancer diagnosis, or deferring essential preventive care because of fear of COVID-19. And there has never been a better time to quit smoking, get your blood pressure under control, make sure that if you have diabetes it’s well-controlled, and get regular physical activity.
10) We can never again be caught so underprepared.
It is inevitable that there will be future outbreaks. What’s not inevitable is that we continue to be so underprepared. The simple truth is that in our increasingly interconnected world, disease spread anywhere is a risk everywhere. If the world is safer, we will be safer here at home.
Future health and economic security can best be protected by changing the way we allocate funds to protect us all from health threats. We have seen the limitations that caps and sequestrations cause for discretionary funding. And we have seen that even mandatory funding doesn’t ensure stable support. We propose a new approach for specific public health programs that are critical to prevent, detect, and respond to health threats. We call this the Health Defense Operations (HDO) budget designation, and it would exempt critical health protection funding from the Budget Control Act spending caps so our public health agencies can protect us.
HDO programs should be required to submit a bypass professional judgment budget to Congress annually. The NIH submits three bypass budgets to Congress every year that explain the true resource needs for cancer, HIV/AIDS, and Alzheimer’s research. Likewise, Congress and the American people must understand exactly what is needed for our public health defense so that Congress can then appropriate the resources required to sustain the public health system we need to keep us safe. This investment can save millions of lives and potentially trillions of dollars. Sustained, baseline funding is the only way we will ensure we are prepared for the next pandemic. Responsible funding means protecting America, and we must also ensure accountability in our spending so that every dollar is used wisely.
Bill Murray is fated to relive the same fate in the classic movie, Groundhog Day. But we can learn from our mistakes. The horror that COVID-19 is spreading around the world can be a wake-up call so that in both the United States and globally we do everything in our power to both tamp down this pandemic and drive down the risk of future epidemics and pandemics. By investing in public health protection, we will honor those lost to this pandemic and protect those at risk from the next.
Dr. Tom Frieden is Senior Fellow for Global Health and the Council on Foreign Relations and President and Chief Executive Officer of Resolve to Save Lives, an initiative of the global health organization Vital Strategies.0 LIKES SHARE
During the 2014-2016 Ebola epidemic, the CDC produced a weekly dashboard of the most important interventions, objectively grading each in every affected country as red, yellow or green. For Ebola, interventions were in five domains: command and control, surveillance and epidemiology, case management (including laboratory testing), essential health services, and effective communication.
The dashboard focused attention on interventions most likely to stop the epidemic. With COVID-19, the same five domains are essential. Two additional domains to fight COVID-19 are physical distancing and providing social and economic support. Here’s a starter set of 10 areas to be tracked both nationally and in every state and community:
A well-organized emergency management system with empowered incident managers aligned with political leaders.
Testing available for every patient with pneumonia within four hours, every symptomatic person within 12 hours, and capacity for drive-through testing.
Start contact tracing within hours of case identification; identify contacts for >95 percent of cases, track >95 percent of contacts, test 100 percent of symptomatic contacts, and monitor >95 percent of quarantined contacts for 14 days. This is an enormous undertaking, and both trained people and practical digital tools will be essential. China tracked 700,000 contacts — with fewer cases than the U.S. has.
Provide daily briefings with accurate and timely numbers of those infected, ill and deceased, epidemiologic trends and analysis, along with updated guidance from credible spokespeople.
Protect health care workers with policies, training, and personal protective equipment.
Be sure health care systems can safely surge for large numbers of mildly ill patients, a large increase in patients needing intensive care, and patients needing ongoing, non-coronavirus-related care.
Be able to resume targeted or general physical distancing rapidly if needed.
Support nutrition, learning, mental and physical health and well-being, and social needs during isolation and quarantine.
Engage communities, obtaining information through surveys, assessing adherence to physical distancing recommendations, and using findings of these surveys to improve the effectiveness and reduce the disruption of measures taken.
Coordinate with states and localities so guidance and policies are implemented within 24 hours of publication.
You can read my full piece on this topic in The Hill here: https://thehill.com/opinion/healthcare/489887-well-lose-world-war-c-against-the-coronavirus-if-we-dont-fight-the-right1 LIKES SHARE
We all want to open things back up. We can open sooner and safer if we address these six areas: 1) Confirm cases and deaths from the virus have been decreasing steadily for at least 14 days. 2) Ensure healthcare systems are ready in case there is a resurgence so health workers are not harmed and patients can be supported. 3) Implement the 'Box It In' strategy through strategic testing, prompt isolation, contact tracing, and quarantine to keep the virus in a box. 4) Protect those most vulnerable to the virus – older and medically vulnerable people will need to shelter and shield for longer. 5) Have new safety measures in place – open in phases, waiting at least 3 weeks to see if there’s spread between steps, use hand sanitizer, door-front shop pickups, open spaces, physical distancing, and more. We need creativity to re-design for safety in the Era of Covid. 6) Track the virus closely to implement physical distancing again if virus spread could overwhelm our health or public health services.
January 25, 2020 - First Covid Blog
Latest Scientific Developments, and Implications for Novel Coronavirus Prevention and Control
At the end of a busy week of our usual work at Resolve to Save Lives in epidemic prevention and cardiovascular health, combined with requests to advise on and discuss the rapidly evolving coronavirus outbreak, I sat down to read seven scientific articles about coronavirus that had come out in the past day. These give us more information than we’ve ever had, but leave many key questions unanswered. Our understanding of nCov2019 is rapidly evolving – with new information nearly every hour. These findings can be revised or reversed - early in an outbreak, there's a "fog of war" reality. The first case in the epi-curve that was just published (see Figure) was from December 1, and there was no uptick in cases until around December 20, with the first alert reported on December 31 – a relatively rapid reporting interval.
Here’s a quick summary of the key findings from the scientific publications:
It’s now highly likely that, as suspected, the ancestral source is bats and the first location may have been the wet market in Wuhan – detailed genetic analysis as well as the largest epidemiological investigation published to date show that 27 of 41 initial cases had exposure to the market. As noted, this virus and bat coronaviruses are close relatives. (Why are bats the cause of so many bad pathogens for people? They are mammals and live in huge cities... sound familiar?)
This coronavirus behaves somewhat like SARS, which it resembles genetically, but is much less deadly, and possibly more infectious. In particular, it seems to attack the lower respiratory tract, because of receptor binding to ACE2, which is found predominantly in the lung. Symptoms are mostly related to the lung, and x-rays show viral pneumonia. The virus, which is an RNA virus prone to replication errors, may well mutate and evolve in the coming months and years.
Superspreader events – one individual or event resulting in many infections – are likely to occur or to have occurred, as they did with both SARS and MERS.
Nosocomial transmission (spread within health care facilities), which was a major source of spread for MERS and SARS, has occurred and remains a major risk for nCov2019 – and is also a major intervention point for control. (The link above is to a familial cluster which may have started with nosocomial transmission. Although this is not proven, it’s clear that nosocomial transmission is occurring.)
From a meticulous description of a family outbreak, it appears that the incubation period may be 3-6 days, at least for some patients, and it is proven that the disease can spread within a household.
One of the leading global units that models disease outbreaks estimates that the reproductive rate, Ro, has been 2.6 (estimated range 1.5-3.5) so far. This is a high number that is consistent with rapid spread observed. The authors note that Ro can decrease as control measures are implemented, but note: “Whether the reduction in transmission is sufficient to reduce R to below 1 – and thus end the outbreak – remains to be seen.”
At least one hospital in Wuhan has begun a clinical trial of antiviral agents.
In addition, public reports indicate increasing recognition of cases in many areas of China, and cases are being identified in an increasing number of countries on several continents. It’s possible that nCov2019 will spread more readily than SARS did, although we don’t know that yet.
What does that all mean?
We still don’t know how infectious the disease is and will remain, but it certainly has been infectious.
We still don’t know the denominator – how many people are infected, what proportion don’t have symptoms (although some are without symptoms, including a 10-year-old child), what proportion have mild illness – so we still don’t know the case fatality rate. However, at this point it appears likely that the mortality rate is lower than it was for SARS (11% for SARS vs. 3-4% so far for nCov2019 – 25 deaths out of 835 diagnosed patients initially, although some of those 835 may die, and the total number infected is undoubtedly much higher than 835, hence the actual mortality rate is likely to be lower, and perhaps far lower).
What should be done?
For most people in the US, nothing different. Wash your hands regularly. Cover your mouth and nose when you cough or sneeze. Don’t go to Wuhan, and consider other travel to China carefully – discuss with your doctor. (For staff in China – work from home to the greatest extent possible, avoid crowds and, if possible, avoid health care facilities unless you’re sick.)
Meticulous infection control in hospitals in China and other areas with infected patients, including rapid detection and isolation of patients with cough, respiratory protection, gloves, disinfection, and the other strategies that controlled SARS and MERS in hospitals. This will protect health workers and decrease the amplification of spread of the virus.
Get more epidemiologic information. How many episodes of nosocomial transmission have there been? What has been studied for each? There’s a big difference if the virus has been spreading from high-risk, aerosol-generating procedures such as sputum induction and bronchoscopy, as opposed to spread in waiting rooms and through other casual contact. Have there been superspreader events? For each recognized outbreak with transmission links, what are the most likely modes of spread and what control measures have been tried, with what effect?
Intensive laboratory work, including testing symptomatic patients (and, in some special studies, contacts), developing serological tests, and collecting multiple virus specimens to monitor for genetic changes.
Establish additional sentinel sites in China to determine what proportion of people both with and without symptoms who attend health care facilities are infected.
Each country should review its ability to find, stop, and prevent coronavirus cases
In the medium term, decide whether live markets should be regulated far more strictly, or closed completely. This won’t change the current outbreak, but allowing the current arrangement to continue, which leads to outbreaks, is not a responsible option.
Dr. Tom Frieden (www.DrTomFrieden.net) is former director of the US Centers for Disease Control and Prevention, and former commissioner of the New York City Health Department. He is currently president and CEO of Resolve to Save Lives, a global non-profit initiative of Vital Strategies, working with countries to prevent 100 million deaths and make the world safer from epidemics. Twitter @DrTomFrieden.
Links to articles cited and linked above:
A Novel Coronavirus from Patients with Pneumonia in China, 2019, New England Journal of Medicine
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, The Lancet
Another decade, another coronavirus, New England Journal of Medicine
Coronavirus infections, more than just the common cold, JAMA
A Novel Coronavirus Emerging in China – Key Questions for Impact Assessment, New England Journal of Medicine
Transmissibility of 2019-nCoV, Imperial College.
Last updated
Was this helpful?

